4950
Developing pre-biopsy multiparameteric MRI based risk calculator for predicting prostate cancer in men with PSA 4-10 ng/ml1Department of NMR and MRI Facility, All India Institute of Medical Sciences, New Delhi, Delhi, India, 2Department of Radiodiagnosis, King George's Medical University, Lucknow, India, 3Department of Urology, All India Institute of Medical Sciences, New Delhi, Delhi, India, 4Division of Biostatistics and Epidemiology, Department of Biomedical Sciences, Texas Tech University Health Sciences Center, El Paso, Texas, TX, United States, 5Department of Radiodiagnosis, All India Institute of Medical Sciences, New Delhi, New Delhi, India, 6Department of Pathology, All India Institute of Medical Sciences, New Delhi, New Delhi, India
Synopsis
Risk calculators have traditionally utilized PSA values in addition to the clinical variables to predict risk assessment of prostate cancer (PCa). For the first time, we aimed to develop pre-biopsy mpMRI based simple risk score (RS) and a predictive model in predicting the risk of PCa in men with clinically challenging value of PSA (4-10 ng/ml) if a TRUS-guided biopsy is performed. The predictive model and developed simplistic 6-point mpMRI score based risk calculator in this study could be routinely used in predicting PCa in clinical management for men with PSA 4-10 ng/ml.
Abstract
Introduction: Risk calculators have traditionally utilized PSA values in addition to the clinical variables to predict risk assessment of prostate cancer (PCa). In these calculators, PSA has been a major contributor to calculate the risk for PCa. However, elevated PSA is not PCa specific, on the other hand there is approximately 25% chance of occurrence of PCa in men with gray zone of PSA (4-10 ng/ml). Recently, multiparametric MRI (mpMRI) has shown potential with increased specificity in detecting clinically significant PCa. 1, 2 Inclusion of mpMRI findings could provide a robust risk calculator for predicting PCa. In this work, we aimed to develop pre-biopsy mpMRI based simple risk score (RS) and predictive model in predicting the risk of PCa in men with clinically challenging value of PSA (4-10 ng/ml) if a TRUS-guided biopsy is performed.
Methods: A total of 148 patients underwent pre-biopsy mpMRI examination. Of the 148 patients, 11 patients were excluded because of motion artefacts/ distortions. Thus, 137 patients formed the study group. The inclusion criteria were: men above the age of 40 years with PSA 4-10 ng/ml; the patient must be a potential candidate for PCa treatment; and signed informed consent. The exclusion criteria were: patients with contraindication for MRI; and patients with known causes for elevated PSA. All patients underwent pre-biopsy MR evaluations at 1.5 Tesla MR scanner (AVANTO, Siemens Health Care, Germany) using an endorectal surface coil (Medrad Inc., Pittsburgh, PA) in combination with a pelvic phased array coil. Following scout images, T1-weighted images in transverse plane and T2-weighted images in three orthogonal planes, MRSI and DW-MRI were acquired. The parameters used for MRSI were as follows: TR = 1300 ms, TE = 120 ms, voxel size = 5 x 5 x 5 mm3, averages = 3, total acquisition time = 17 min. Single shot EPI pulse sequence was used for diffusion weighted (DW) images. Slice positions of DW-MRI were matched with T2-weighted images. Five different b values (0, 250, 500, 750 and 1000 s/mm2) were used to acquire different diffusion-weighted images (TR = 3000 ms, TE = 96 ms, 5 mm slice thickness without interslice gap, number of averages = 2, bandwidth = 1500 Hz). A cut-off value of metabolite ratio [Citrate/(Choline+Creatine)] ratio < 1.2 and cut-off value of ADC < 1.17 x10-3 mm2/s were used to predict malignancy from our earlier study. 3 A p < 0.05 was considered to indicate statistical significance. An equation model and simple risk calculator were developed for the first time using novel approach by applying receiver operating characteristics (ROC) curve analysis and multivariable logistic approach. Statistical analyses were performed using commercially available software (STATA 13, STATA Corp., College Station, Texas, USA).
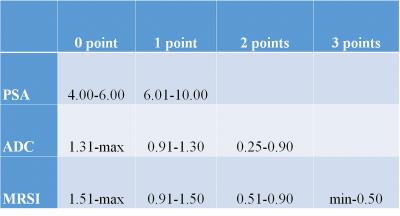
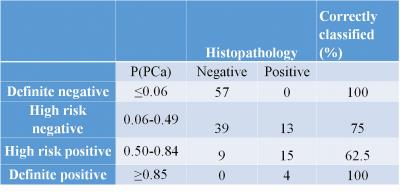
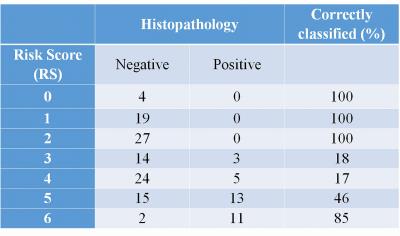
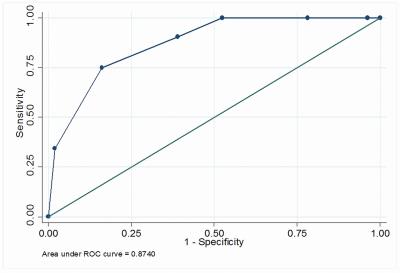
Results: A 6-point mpMRI score was generated, which is very simple in calculating the risk of PCa. Table 1 shows the identified ranges of PSA, ADC and metabolite ratio to calculate RS for the individual subject. For example, the score for a patient with > 6 PSA (1 point), a ADC of 0.25 (2 points), a metabolite ratio of 0.55 (2 points) would be 5 while a patient with > 6 PSA (1 point), the ADC of 1.35 (0 points), the metabolite ratio of 1.55 (0 points) would receive a score of 1. The developed predictive model was internally validated and performance is provided in Table 2 while the internal validation of developed 6-point RS model is provided in Table 3. RS was found to be highly predictive for PCa (odds ratio - OR = 3.74, 95%CI: 2.24-6.27, area under the curve (AUC) = 0.87, Figure 1).
Discussion: Selection of appropriate treatment for the aggressive prostatic disease is still a clinical challenge. A simple and user friendly risk calculator can help clinicians and patients to assess the risk for PCa and choosing appropriate therapy. The first PCa risk calculator, prostate cancer preventions trial (PCPT) was published in 2006. 4 Majority of previous risk calculators utilized PSA based derivatives in addition to patient’s clinical details. 4, 5 We developed a novel mpMRI based risk calculator to predict the risk of PCa. Internal validation of the developed models was evaluated and found to be highly satisfactory. We suggest to validate the developed risk calculator externally and prospectively by conducting a larger study with a long follow-up.
Conclusion: The predictive model and developed simplistic 6-point mpMRI score based risk calculator in this study could be routinely used in predicting PCa in clinical management for men with PSA 4-10 ng/ml.
Acknowledgements
No acknowledgement found.References
1. Hoeks CM, Barentsz JO, Hambrock T, et al. Prostate cancer: multiparametric MR imaging for detection, localization, and staging. Radiology 2011; 261: 46-66.
2. Turkbey B, Brown AM, Sankineni S, et al. Multiparametric prostate magnetic resonance imaging in the evaluation of prostate cancer. CA Cancer J Clin 2016; 66: 326-36.
3. Dwivedi DK, Kumar R, Bora GS, et al. Stratification of the aggressiveness of prostate cancer using pre-biopsy multiparametric MRI (mpMRI). NMR Biomed 2016 ;29:232-38.
4. Thompson IM, Ankerst DP, Chi C, et al. Assessing prostate cancer risk: results from the Prostate Cancer Prevention Trial. J Natl Cancer Inst 2006; 98: 529-34.
5. D'Amico AV, Whittington R, Malkowicz SB, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 1998; 280: 969-74.
Figures