4948
3D Virtual Reality Models Created from MRI data for Pre-operative Evaluation of Renal Cancer1Bernard and Irene Schwartz Center for Biomedical Imaging, Center for Advanced Imaging Innovation and Research, Department of Radiology, New York University School of Medicine, New York, NY, United States, 2Department of Urology, New York University School of Medicine, New York, NY, United States
Synopsis
The objective of this study was to create patient-specific 3D virtual reality kidney cancer models and to evaluate pre-operative planning decisions made using these models. Virtual 3D models were compared to 3D printed models. These models may alter the surgical plan, and could promote both nephron-sparing surgery and preservation of healthy parenchyma, as surgeons gain a better visualization of the size and location of a tumor in relation to normal tissue and vital structures.
Introduction
Kidney cancer or renal cell carcinoma (RCC) is a common cancer, accounting for approximately 3.5% of all malignancies.1,2 The standard of care for RCC is surgical resection with minimally invasive partial nephrectomy the treatment of choice for localized tumor.1 In addition, current guidelines emphasize nephron-sparing surgery for all anatomically amenable T1 renal tumors.3 Clinical decisions regarding surgical approach are typically based on review of 2D images or 3D reconstructions, as the decision to perform a partial nephrectomy and which approach to take is a complex interaction between various patient factors, the anatomic relationship of the tumor with other structures, and the location of the tumor within the kidney.4,5 We have previously shown that pre-operative 3D printed models of renal mass are valuable tools that facilitate pre-operative planning by allowing surgeons to assess both tumor complexity and the relationship of the tumor to major anatomic structures such as the renal vasculature and collecting system.6,7 However, 3D printed models are expensive and difficult to generate, therefore printing may not always be feasible. Augmented reality (AR), a technology that has recently become available to the general public, enables one to visualize 3D models as digital objects in the real world; and it is believed this new technology may help to plan and guide surgical interventions.8 The objective of this study was to create virtual renal cancer models and to evaluate pre-operative planning decisions made using these virtual models.Methods
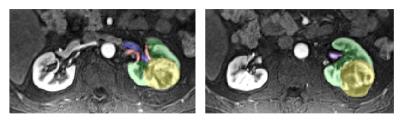
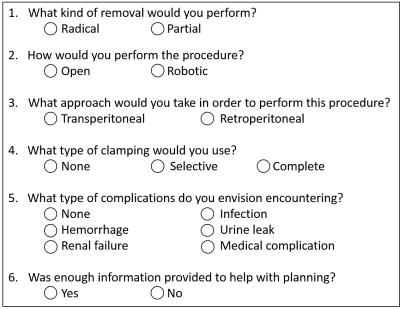
Ten renal malignancy cases with Nephrometry scores ranging from 6a-10p were retrospectively selected. A 3D post-contrast fat-suppressed gradient-echo T1 weighted sequence with a spatial resolution of 1.4 mm x 1.4 mm x 2mm was used to generate the 3D models. Image segmentation of the kidney, tumor, renal artery, renal vein, and collecting system was performed (Mimics, Materialise, Leuven, Belgium) (Figure 1). Anatomical regions of interest were smoothed to reduce the pixelated appearance and converted to .STL for printing and .OBJ format for viewing in AR. High-fidelity, patient-specific 3D renal tumor models were imported to the Microsoft HoloLens AR headset and were also 3D printed in multiple colors (Connex 500, Stratasys, Eden Prairie MN). Renal malignancy cases were anonymized and were reviewed by two attending urologists, each with 12 years of experience, in a random order in three different settings: 1) imaging, 2) imaging and 3D printed model, and 3) imaging and virtual model. A questionnaire was completed after all three scenarios to assess pre-surgical planning decisions (Figure 2). Pre-operative planning decisions were compared, and any change between the presumed approach and actual surgical intervention was recorded. The surgeons were also asked to rank their preferred method of data visualization for each case and to give comments regarding model preference.Results
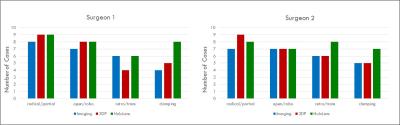
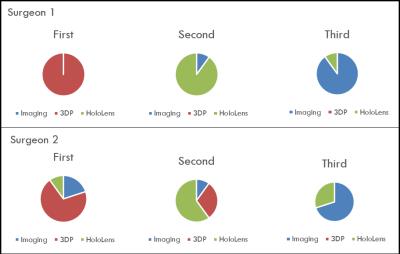
Visual assessment demonstrated that the virtual reality models accurately depict the anatomy and closely resemble both computer and 3D printed models (Figure 3). Results for the surgical planning decisions are shown in Figure 4. Both physicians reported that both 3D printed and virtual reality models helped with regards to surgical approach for partial nephrectomy. Virtual models were preferred more than the image analysis on PACS, however were not preferred over the 3D printed models. Rankings for the models are shown in Figure 5.Discussion/Conclusion
A method for viewing patient-specific 3D renal cancer models in AR has been successfully implemented and trialed on two surgeons. Initial testing demonstrates that virtual models give surgeons an improved understanding of the tumor anatomy and may alter surgical planning decisions. The surgeons tended to prefer the 3D printed models over the virtual models, stating that the preference may have been due to the learning curve associated with using the HoloLens device. In addition, the surgeons believe that having an AR model may be the most beneficial if the AR kidney model could be co-registered to the actual kidney for robotic or laparoscopic cases at the time of surgery. Future, outcome based studies may help to determine the preferred method of MRI data visualization for renal cancer models as well as the impact of pre-operative 3D models on surgical outcomes and patient care.Acknowledgements
This work was supported by the Center for Advanced Imaging Innovation and Research (www.cai2r.net), a NIBIB Biomedical Technology Resource Center (NIH P41 EB017183).References
1. Chen DY, Uzzo RG. Optimal management of localized renal cell carcinoma: surgery, ablation, or active surveillance. J Natl Compr Canc Netw. 2009:7(6):635-42.
2. Sivarajan G, Huang WC. Current Practice Patterns in the Surgical Management of Renal Cancer in the United States. Urol Clin N Am. 2012; 39: 149–160.
3. Gandaglia G, Ravi P, Abdollah F, Abd-El-Barr AE, Becker A, Popa I, Briganti A, Karakiewicz PI, Trinh QD, Jewett MA, Sun M. Contemporary incidence and mortality rates of kidney cancer in the United States. Can Urol Assoc J. 2014;8(7-1):247-21.
4. Broughton, Clark PE, Barocas DA, Cookson MS, Smith JA Jr, Herrell SD, Chang SS. Tumour size, tumour complexity, and surgical approach are associated with nephrectomy type in small renal cortical tumours treated electively. BJU Int. 2012 Jun;109(11):1607-13.
5. Funahashi Y, Murotani K, Yoshino Y, Sassa N, Ishida S, Gotoh M. The renal tumor morphological characteristics that affect surgical planning for laparoscopic or open partial nephrectomy. Nagoya J Med Sci. 2015;77: 229-35.
6. Wake N, Chandarana H, Huang WC, Taneja SS, Rosenkrantz AB. Application of anatomically accurate, patient-specific 3D printed models from MRI data in urological oncology. Clin Radiol. 2016 Jun;71(6):610-4.
7. Wake N, Rude T, Huang WC, Stifelman MD, Borin JF, Sodickson DK, Chandarana H. 3D Printed Renal Cancer Models Derived from MRI data: Application in Pre-Surgical Planning. Proc. Intl Soc Mag Reson Med 24 (2016) Singapore.
8. Marescaux J, Diana Michele. Inventing the Future of Surgery. World J Surg. 2015:39:615-22.
Figures