4942
Investigating the role of DCE-MRI, over T2 and DWI, in accurate PIRADS-v2 assessment of clinically significant peripheral zone prostate lesions, as defined at radical prostatectomy1Radiology, Harvard Medical School, Brigham and Women's Hospital, BOSTON, MA, United States, 2Imaging, Dana-Farber Cancer Institute, Boston, MA, United States, 3Radiology, Harvard Medical School, Massachusetts General Hospital, Boston, MA, United States
Synopsis
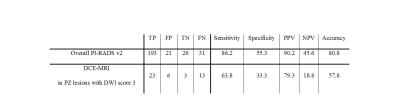
DCE has a secondary role in detecting peripheral zone lesions using PIRADS v2 and is limited to PZ lesion with DWI score of 3. The goals of this study are to determine the frequency with which DCE plays a role changing the final PI-RADS assessment score for PZ lesions, and 2) determine the accuracy of DCE-MRI in upgrading the assessment score . 271 patients with biopsy proven prostate cancer diagnosis, a mp-MRI, and who underwent curative radical prostatectomy were included in the study. DCE played a role only in 16.6% (45/271) of patients and showed sensitivity of 63.8% in upgrading lesions. In conclusion, the added value of DCE to T2-WI and DWI is very limited in diagnosis of csPC.
Introduction
Multiparametric magnetic resonance imaging (mp-MRI) is an important toolin diagnosis and localization of csPC [1], and critical for surveillance, risk stratification, and image guidance for prostate biopsy [1, 2]. In an effort to standardize mpMRIacquisition, interpretation and reporting, Prostate Imaging – Reporting and Data System (PI-RADS) was developed [3]. And the second version (PI-RADS v2) [4], aims to simplify the usage and to improve diagnostic performance of mpMRI. As per PI-RADS v2, in the peripheral zone (PZ), Diffusion weighted Imaging (DWI) is the determinant sequence for scoring unless the lesion has borderline characteristics of a PIRADS score of 3. In such cases a positive DCE upgrades the assessment category to a PI-RADS 4, which corresponds to a csPC [5, 6]. Using a large dataset of radical prostatectomy patients, the goal of this study is to 1) determine the frequency with which DCE plays a role changing the final PI-RADS assessment score for PZ lesions, and 2) determine the accuracy of DCE-MRI in upscoring the assessment score.Methods
This is a retrospective institutional review board approved record-review study of 271 patients with pathologically-proven primary PC who underwent a standard of care e-coil prostate mpMRI at 3T[7], and subsequently underwent radical prostatectomy. Two radiologists, blinded to the pathology, separately performed an overall PI-RADS v2 assessment. A third reader resolved any discrepancies. csPC was defined as Gleason ≥ 7, or Volume ≥ 0.5, or stage ≥ T3a based on pathology results of prostatectomy. Performance characteristics (Sensitivity, specificity, positive/negative predictive values (PPV, NPV)), and diagnostic accuracy of PI-RADS v2 scoring and the secondary role of DCE imaging were calculated.Results
A total of 271 men with mean age of 59 y/o (43-76y) and mean PSA 6.7ng/ml (0.01-38.7) were included. 224/271 (82.6%) had csPC (211 Gleason ≥ 7, 134 Volume ≥ 0.5, 46 stage ≥ T3a) at RP. On mpMRI scans combined, 209 Prominent suspicious lesions were localized in PZ, 31 in transitional zone (TZ), 4 in Central zone, 3 in anterior segment, and in 24 MRI scans no suspicious lesion was reported. Table 1 represents the Performance characteristics and accuracy of PI-RADS v2 in diagnosing csPC. DCE was redundant in 83.4% (226/271, TZ lesions or DWI score other than 3) of patients and only in 16.6% (45/271) of patients, DCE findings impactedPI-RADS v2 scoring. In those cases, DCE was positive in 29 and negative in 16 cases. When DCE findings were compared to the gold standard (pathology Gleason score, volume, and stage),23 cases turned out to be true positive and 6 false positive. Among patients with negative DCE, only 3 cases turned to be true negative and 13 cases were false negative (table 1)Discussion
Our results represents that DCE-MRI is only required in a limited number of cases with considerable false positive rate, which is in line with recent literature [7]. Itehrefore, DCE is not required in most of the cases and could be reserved to only those patients with a score 3 on DWI of prominent PZ lesion. This approach will decrease the costs of MRI, scanning time, as well as contrast related side effects; however it requires onsite/realtime evaluation of images by an expert radiologist, otherwise the patient might have to be return for the second scan [8, 9].Conclusion
The value of DCE-MRI in prostate cancer evaluation, even as a secondary role, is very limited. We encourage obtaining a DCE imaging only in select patients.Acknowledgements
Grant funding provided by U01CA151261 (FMF) , P41 EB015898 (CT, FMF) and DPH403516 (FF, CT).References
1.Turkbey, B., et al., Multiparametric prostate magnetic resonance imaging in the evaluation of prostate cancer. CA Cancer J Clin, 2016. 66(4): p. 326-36.
2.Penzkofer, T., et al., Transperineal in-bore 3-T MR imaging-guided prostate biopsy: a prospective clinical observational study. Radiology, 2015. 274(1): p. 170-80.
3.Bomers, J.G. and J.O. Barentsz, Standardization of multiparametric prostate MR imaging using PI-RADS.Biomed Res Int, 2014. 2014: p. 431680.
4.Weinreb, J.C., et al., PI-RADS Prostate Imaging - Reporting and Data System: 2015, Version 2. Eur Urol, 2016. 69(1): p. 16-40.
5.Barrett, T., B. Turkbey, and P.L. Choyke, PI-RADS version 2: what you need to know. Clin Radiol, 2015. 70(11): p. 1165-76.
6.Hassanzadeh, E., et al., Prostate imaging reporting and data system version 2 (PI-RADS v2): a pictorial review.Abdom Radiol (NY), 2016.
7.Hegde, J.V., et al., Multiparametric MRI of prostate cancer: an update on state-of-the-art techniques and their performance in detecting and localizing prostate cancer. J Magn Reson Imaging, 2013. 37(5): p. 1035-54.
8.De Visschere, P., et al., Dynamic contrast-enhanced imaging has limited added value over T2-weighted imaging and diffusion-weighted imaging when using PI-RADSv2 for diagnosis of clinically significant prostate cancer in patients with elevated PSA. Clin Radiol, 2016.
9.Vargas, H.A., et al., Updated prostate imaging reporting and data system (PIRADS v2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: critical evaluation using whole-mount pathology as standard of reference. Eur Radiol, 2016. 26(6): p. 1606-12.