4912
Quantification of regional lung ventilation in COPD patients: Validation of ventilation-weighted Fourier decomposition-MRI with dynamic fluorinated gas MRI and lung function testing.1Institute of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Center for Lung Research (DZL), Hannover, Germany, 3Clinic of Pneumology, Hannover Medical School, Hannover, Germany
Synopsis
Quantification of regional lung ventilation is of high relevance for lung diseases like chronic obstructive lung disease (COPD) or asthma. Regional ventilation of the lungs in COPD patients was assessed using ventilation-weighted Fourier decomposition-MRI and validated with real-time dynamic fluorinated MRI and lung function test. Strong correlations were found comparing both techniques with each other and with lung function testing which is used for COPD classification.
INTRODUCTION: “Why was this study/research performed? What unsolved problem are you addressing?”
Chronic obstructive lung disease (COPD) is a common chronic lung disease with a high morbidity and mortality. Pulmonary function testing, the current clinical standard for obtaining lung ventilation, is used for grading (GOLD classification) and treatment recommendations, but provides only global information. Thus, techniques for assessment of regional lung function came into focus in order to improve monitoring and clinical management of COPD patients. Pulmonary gas MRI (3He, 129Xe, 19F) have been shown to facilitate evaluation of regional lung ventilation. However, these techniques are time-consuming and cost intensive. In contrast to that, ventilation-weighted Fourier decomposition-MRI (FD-MRI) is cost-efficient and widely available. Thus, aim of this study was to correlate regional fractional ventilation obtained by FD-MRI with dynamic fluorinated gas MRI (19F-MRI) and lung function tests.METHODS: “How did you study this problem?”
The study was approved by the institutional ethical review board and all subjects gave written informed consent. Nine patients with COPD (median age 60 years, median FEV1 63 [51-87,5]%) underwent 1.5T MRI. For ventilation-weighted FD-MRI four coronal slices were acquired in free breathing using a spoiled gradient echo sequence with TE 0.7 ms, TR 3 ms, flip angle 8°, matrix size 128 x 96, field of view 50 x 50 cm, slice thickness 15 mm and a temporal resolution of 288 ms. After applying a non-rigid registration, fractional ventilation maps (FV-FD) were calculated as previously described1,2.
Dynamic 19F imaging was performed with a dedicated coil (Rapid Biomedical) tuned to 59.9 MHz consisting of a transmit Helmholtz coil and a 16 channel phased-array receive coil using a 3D spoiled gradient echo sequence (TE=5.1 ms, TR=12 ms, flip angle=50°, FOV=50x50x20 cm³, matrix size=64x64x6, bandwidth=140 Hz/pixel, GRAPPA factor=2). Each patient inhaled 30l of a mixture of 79% fluorinated gas (C3F8) and 21% oxygen via a closed face mask. Afterwards, while inhaling 100% oxygen, wash-out dynamics were assessed. Washout time in number of breaths (washout[#breaths]) and fractional ventilation (FV-19F) were calculated as previously described3-5.
FD-MRI and 19F-MRI were anatomically matched using a landmark driven algorithm, and only corresponding slices with an overlap of > 90% were selected for evaluation. For comparison with the current clinical standard, all patients underwent a lung function test. The obtained parameters were correlated with each other using Spearman’s correlation coefficient.
RESULTS: “Report the data and statistical analyses”
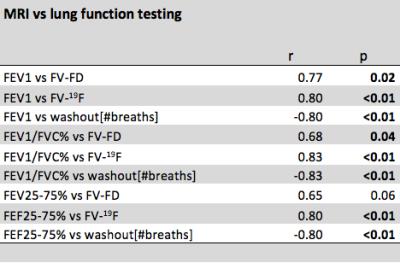
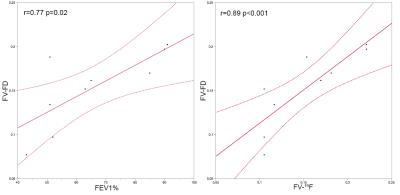
All COPD patients
completed the MRI exam without any side effects. FV-FD, FV-19F and
washout[#breaths] correlated with lung function tests as shown in figure 1 and
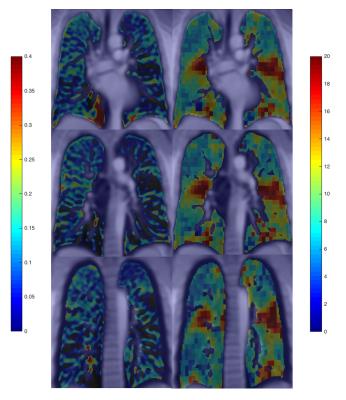
2. Exemplary corresponding maps of
ventilation-weighted FV-FD and FV-19F are shown in figure 3.
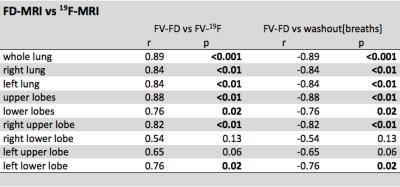
Correlations of regional fractional ventilation measured by FD and dynamic fluorinated gas MRI are shown in figure 4. Both
methods showed strong correlations on a global level (r=0.89 p<0.001) as
well as on a regional level dividing the lung in upper/lower lobes or right and
left lung. On a lobar level also correlations between ventilation-weighted
FV-FD and FV-19F were observed.
DISCUSSION: “How do you interpret the the data?”
Ventilation-weighted Fourier
decomposition-MRI can measure impaired regional
lung ventilation due to emphysema and air trapping in patients with COPD.
Ventilation-weighted FV-FD and FV-19F show positive correlation to
FEV1, FEV1/VC and FEF25-75%, which are used in clinical routine to grade the severity
of COPD (GOLD classification6). These MRI techniques can be carried
out in free breathing and are radiation free. In addition, FD-MRI is less
time-consuming, less expensive and needs no additional hardware, which
facilitates a broad use of ventilation-weighted Fourier
decomposition-MRI on 1.5T scanners today.
CONCLUSION: “What is the relevance to clinical practice or future research?”
Ventilation-weighted Fourier
decomposition-MRI in free breathing allows quantification of regional lung
ventilation comparable to pulmonary gas MRI at lower costs and a broader
availability and thus could add value to the
current clinical lung function test improving diagnosis and monitoring of COPD
patients.
Acknowledgements
This work was supported by the German Centre for Lung Research (DZL), Regenerative Biology and Reconstructive Therapies (REBIRTH) and Fritz-Behrens-Stiftung, Hannover.References
1. Bauman G, Puderbach M, Deimling M, et al. Non-contrast-enhanced perfusion and ventilation assessment of the human lung by means of fourier decomposition in proton MRI. Magnetic resonance in medicine 2009;62(3):656-664.
2. Voskrebenzev A, Gutberlet M, Becker L, et al. Reproducibility of fractional ventilation derived by Fourier decomposition after adjusting for tidal volume with and without an MRI compatible spirometer. Magn Reson Med 2015; 76(5):1542–1550.
3. Halaweish AF, Moon RE, Foster WN, et al. Perfluoropropane gas as a magnetic resonance lung imaging contrast agent in humans. Chest. 2013;144(4):1300–1310.
4. Ouriadov AV, Fox MS, Couch MJ, et. al. In vivo regional ventilation mapping using fluorinated gas MRI with an x-centric FGRE method. Magn. Reson. Med. 2015;74(2):550–557.
5. Gutberlet M, Kaireit T, Voskrebenzev A, et al. Real-time dynamic fluorinated gas MRI in free breathing for mapping of regional lung ventilation in patients with COPD and healthy volunteers using a 16 channel receive coil at 1.5T. Proc. Intl. Soc. Mag. Reson. Med. 24 (2016): 1140 .
6. Rabe KF, Hurd S, Anzueto A, et al. Global
strategy for the diagnosis, management, and prevention of chronic obstructive
pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532-55.
Figures