4902
Differentiation of thymic hyperplasia from thymic tumors with MR quantitative fat fraction technique in adulthood1Department of Radiology, Tangdu Hospital, Fourth Military Medical University, Xi'an, People's Republic of China, 2MR Research China, GE Healthcare China, Beijing, China
Synopsis
MRI estimated proton density fat fraction (MRI-PDFF) gives quantitative information of fat deposition in soft tissue. This study retrospectively evaluate the effectiveness of MRI-PDFF for distinguishing thymic hyperplasia from thymic tumors. As a conclusion, a significant higher mean fat fraction values were found in thymic hyperplasia compared to thymic tumors. MRI-PDFF technique could be used to differentiate thymic hyperplasia from thymic tumors before treatment.
Target audience Researchers and clinicians interested in mediastinal tumor imaging, with a particular interest in chemical-shift magnetic resonance (MR) imaging.
Introduction Recently, the use of magnetic resonance (MR) in clinical practice for mediastinum disease evaluation has considerably increased due to improvements and standardization of thoracic protocols [1]. Chemical shift imaging are helpful in tissue characterization and present advantages over conventional MRI in differentiating thymic hyperplasia from thymic tumors [2, 3]. However, chemical-shift MR imaging could have some limitations as a modality for the differentiation of normal or hyperplastic thymus from anterior mediastinal tumors, with a lower accuracy than reported previously[2]. A recent MR technique - MRI estimated proton density fat fraction (MRI-PDFF) gives quantitative information of fat deposition in tissue [4].
The purpose of this study is to retrospectively evaluate the effectiveness of MRI-PDFF for distinguishing thymic hyperplasia from thymic epithelial tumors and thymic lymphoma.
Methods This retrospective study was approved by the Ethics Committee and informed consents were obtained from all participants. Between November 2015 and September 2016, forty-seven subjects (26 men, 21 women; age range, 16–76 years) were divided into thymic hyperplasia group (n=9), thymic epithelial tumors group (n=28) and thymic lymphoma group (n=10).
All the MR examinations of the thorax were performed using a 3.0-T whole-body system (MR750, GE Healthcare, Milwaukee, WI) with a 40-mT/m maximum gradient capability and a 8 channel body coil. Conventional thorax MRI and IDEAL-IQ (iterative decomposition of water and fat with echo asymmetry and least-squares estimation quantization) sequence were performed during the same examination.
A freehand ROI was placed on the thymic lesion parts on the fat fraction images by an experienced radiologist. Final fat fraction (%) was calculated by averaging of the value from 3 measurements (Fig 1 a2,b2). Mean fat fraction values were compared for the differences among thymic hyperplasia, thymic epithelial tumors and thymic lymphoma groups using one-way ANOVA, and further post hoc multiple comparisons were performed with Bonferroni test (equal variances assumed) and Dunett's T3 test (equal variances not assumed).
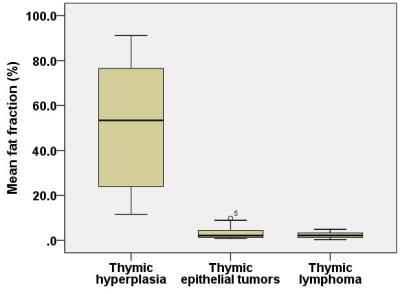
Results Mean fat fraction values tended to be higher in the thymic hyperplasia (52.36 ± 30.2 %, P<0.001, Fig 2), while no significant differences were found between thymic epithelial tumors and thymic lymphomas (3.07 ± 2.47 % and 2.43 ± 1.57 % respectively, P > 0.05, Fig 2).
Discussion This study suggested that fat fraction values based on MRI-PDFF technique could be used to differentiate thymic hyperplasia from thymic tumors. We detected significant differences in mean fat fraction values between thymic hyperplasia and thymic tumors in adult cohort. In addition, and no overlapping values between thymic hyperplasia and thymic tumors were demonstrated in current study, hence, MRI-PDFF seems to be preferable for the differentiation of the thymic lesions compared to the dual-echo chemical-shift MR imaging [3].
Conclusions MRI-PDFF technique provide accurate fat quantitative parameters and can be used to differentiate thymic hyperplasia from thymic tumors before treatment.
Acknowledgements
We thank other consultants of Department of Radiology of Tangdu hospital for their help in this study. We also thank Tangdu hospital for providing related instruments for this study.References
[1] Priola AM, Gned D, Veltri A, et al. Chemical shift and diffusion-weighted magnetic resonance imaging of the anterior mediastinum in oncology: Current clinical applications in qualitative and quantitative assessment. Crit Rev Oncol Hematol[J], 2016,98:335-357.
[2] Priola AM, Priola SM, Ciccone G, et al. Differentiation of rebound and lymphoid thymic hyperplasia from anterior mediastinal tumors with dual-echo chemical-shift MR imaging in adulthood: reliability of the chemical-shift ratio and signal intensity index. Radiology[J], 2015,274(1):238-249.
[3] Inaoka T, Takahashi K, Mineta M, et al. Thymic hyperplasia and thymus gland tumors: differentiation with chemical shift MR imaging. Radiology[J], 2007,243(3):869-876.
[4] Reeder SB, Cruite I, Hamilton G, et al. Quantitative Assessment of Liver Fat with Magnetic Resonance Imaging and Spectroscopy. J Magn Reson Imaging[J], 2011,34(4):spcone.
Figures