4897
Multicentre repeatability of ADC estimates from diffusion weighted (DW) MRI in lung cancer: influence of segmentation methodology and statistical descriptor1Radiotherapy and Imaging, The Institute of Cancer Research, Surrey, United Kingdom, 2Centre for Imaging Sciences, Division of Informatics Imaging & Data Sciences, University of Manchester, MANCHESTER, United Kingdom, 3Department of Biomedical Sciences, Humanitas University, Rozzano (Milano), Italy
Synopsis
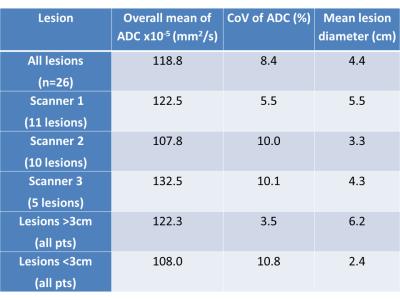
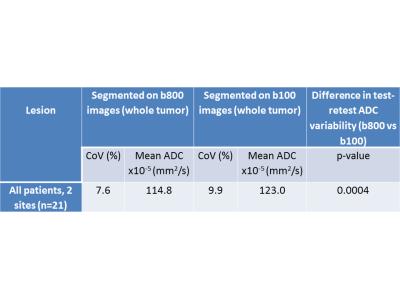
Using a multi-platform diffusion weighted MRI protocol in lung tumors, apparent diffusion coefficient (ADC) repeatability was well below the change expected for treatment response. ADC coefficients of variation (CoV) varied depending on lesion size and segmentation methodology (range 2.6-10.8%; three times greater for lesions >3cm than lesions<3cm). Performing tumor segmentation on high-b-value images produced lower, more repeatable ADC estimates than if segmenting on low-b-value images. Using median versus mean statistical descriptors for signal averaging prior to ADC calculation did not affect ADC quantitation or repeatability.
INTRODUCTION
AIM
To assess the impact of different segmentation methodologies and statistical descriptors on absolute ADC estimates and their repeatability in a multi-centre test-re-test study of lung tumors.
METHOD
Across 3 institutions, 21 informed, consenting patients with lung tumors >2 cm in diameter (n=26 lesions) were scanned on two occasions >1 hour and <1 week apart. Acquisitions were performed during free breathing, using 2 anterior phased-array body coils on the following 1.5T platforms: Siemens; Philips; and GE. Sequence parameters were: single-shot echo-planar DW-imaging, FoV=380x273mm, acquired matrix=128x92, pixel=3x3mm, parallel imaging factor=2, PE direction=AP, TR=8500ms, TE=72ms, short time inversion recovery (STIR) fat suppression, three scan trace, single-spin-echo, b=100, 500, 800 s/mm2, 25 to 40 slices, slice thickness=5mm, NSA=1.
Whole tumor segmentation was performed for all lesions >2cm in diameter using a previously validated region growing segmentation methodology3. Regions of interest were generated by an experienced radiologist on the low b (=100 s/mm2) and high b (=800 s/mm2) images and ADC was calculated using log-linear fit of signal intensity with increasing b-value (ADEPT, ICR, UK).
The median ADC (ADCmed) values were compared using the paired sample t-test when segmentation was done on the b100 vs b800 images at the first time-point. In addition, coefficients of variation (CoV) were recorded for test-retest ADCmed values measured for: All lesions; lesions >3cm; and lesions according to scanner used (using b800 images for segmentation).
In 10 patients (11 lesions) at one scanning site, each diffusion-weighted gradient was applied sequentially in 3 orthogonal directions, over 4 acquisitions, to generate 12 intensity values at each b-value. From the multiple acquisitions, mean and median signal intensity were calculated per-voxel, using a purpose written algorithm within PyOsirix software. The resulting mean and median images for each b-value were used to generate ADC maps, using log-linear fit of signal decay with increasing b-value [PyOsirix, ICR, UK]. The ADC values generated using the two signal averaging techniques were compared using the paired sample t-test and the effect on ADC repeatability assessed with the concordance correlation coefficient (CCC) between techniques, plus CoV for each technique.
RESULTS
ADC values and their CoVs for all lesions, for lesions > 3cm and for different scanners are given in Table 1. Tumor volumes generated using the b100 images (mean =119.5ml) were 29.8% larger than those on the same image slices on the b800 images (mean =91.8ml) (p=0.005). The ADCmed values generated when segmenting tumor on the b800 images was significantly lower than when using the b100 images (Table 2). The CoV for ADC values from the two segmentation methods was 9.9% (b100) and 7.6% (b800).
There was no significant difference in ADC values generated using the mean averaged compared with the median images at each b-value (p=0.15). Similarly, the ADC test-retest coefficients of variation were very similar using the two techniques - CoV was 5.2 % (95%CI 3.8 to 8.4) [LoA 15.6 to -13.5%] for the ‘median’ images, compared with 4.8 % (95%CI 3.5 to 7.8) [LoA 14.3 to -12.5%] for the ‘mean’ images. The CCC for the two techniques (ADC calculated from mean averaged acquisitions compared with median) was 0.98 (95% CI 0.97-0.99).
DISCUSSION AND CONCLUSION
Multi-platform DW-MRI produced robust ADC estimates that have excellent repeatability for measuring treatment response in lung cancer. Superior repeatability and lower ADC is obtained when segmenting on high-b compared with low-b images, due to the exclusion of surrounding pulmonary atelectasis when using the former (Figure 1, Table 2). ADC repeatability was three times better when lesions >3cm in diameter only were included, due in part to the greater effect of respiratory motion on smaller lesions. The repeatability of ADCmed values obtained across scanners is well below the change in ADC expected following successful therapy1. Use of the median averaged acquired images did not affect ADC quantitation or repeatability.Acknowledgements
We acknowledge CRUK and EPSRC support to the Cancer Imaging Centre at ICR and RMH in association with MRC & Dept of Health C1060/A10334, C1060/A16464 and NHS funding to the NIHR Biomedicine Research Centre and the Clinical Research Facility in Imaging. M.-V. P. was funded by EORTC Innovative Medicines Initiative Joint Undertaking under grant agreement number 115151.References
1. Chen L, Zhang J, Bao J, Zhang L, Hu X, Xia Y, et al. Meta-analysis of diffusion-weighted MRI in the differential diagnosis of lung lesions. Journal of magnetic resonance imaging : JMRI. 2013;37(6):1351-8.
2. Jerome NP, Orton MR, d'Arcy JA, Feiweier T, Tunariu N, Koh DM, et al. Use of the temporal median and trimmed mean mitigates effects of respiratory motion in multiple-acquisition abdominal diffusion imaging. Physics in medicine and biology. 2015;60(2):N9-N20.
3. Bernardin L, Douglas NH, Collins DJ, Giles SL, O'Flynn EA, Orton M, et al. Diffusion-weighted magnetic resonance imaging for assessment of lung lesions: repeatability of the apparent diffusion coefficient measurement. European radiology. 2014;24(2):502-11.
Figures