4895
Comparison of the Capability for Quantitative Distinguishing Malignant from Benign Pulmonary Nodules among Dynamic First-Pass CE-Perfusion ADCT and MRI and FDG-PET/CT1Division of Functional and Diagnostic Imaging Research, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 2Advanced Biomedical Imaging Research Center, Kobe University Graduate School of Medicine, Kobe, Japan, 3Division of Radiology, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 4Center for Medical Research and Development, Toshiba Medical Systems Corporation, Otawara, Japan, 5Center for Radiology and Radiation Oncology, Kobe University Hospital, Kobe, Japan
Synopsis
Quantification of perfusion parameter from dynamic CE-perfusion MRI at 3T system may be more difficult than that at 1.5T system, and contrast media concentration may have larger influence to measurement error of perfusion parameter on a 3T system. We hypothesized that a bolus injection protocol with appropriately small contrast media volume can provide accurate pulmonary perfusion parameter on dynamic CE-perfusion MRI at a 3T system. The purpose of this study was to determine the appropriate contrast media volume for quantitative assessment of dynamic CE-pulmonary MRI, when compared with dynamic CE-area-detector CT (ADCT) for quantitative evaluation of perfusion within whole lung.
Introduction
Pulmonary nodules are caused by a variety of conditions, ranging from benign granulomas to operable primary malignant lung nodules. Ideally, the goal of diagnosis and management is to promptly bring to surgery all patients with operable malignant nodules while avoiding unnecessary thoracotomy for patients with benign lesions. Therefore, it is important to differentiate malignant from benign solitary pulmonary nodules in the least invasive manner and to make as specific and accurate diagnoses as possible. In the last decade, diagnostic capability of dynamic first-pass CE-MRI with ultra-short TE has been suggested as higher than that of dynamic CT, PET or PET/CT (1-3). Since 2007, area-detector CT (ADCT) has been clinically installed, and demonstrated that dynamic first-pass perfusion had better potential for diagnosis of pulmonary nodule as compared with semi-quantitatively analyzed dynamic first-pass CE-MRI with ultra-short TE and PET/CT (4). However, no one directly compare diagnostic capability for nodule differentiation among dynamic first-pass CE-perfusion ADCT and MRI with ultra-short TE analyzed by same mathematical method and FDG-PET/CT.
We hypothesized that dynamic first-pass CE-perfusion ADCT and MRI with ultra-short TE applied the same mathematical model have better potentials for differentiation of malignant from benign nodules than FDG-PET/CT.
The purpose of this study was to compare the capability for differentiating malignant from benign nodules among quantitatively assessed dynamic first-pass CE-perfusion ADCT and MRI with ultra-short TE and FDG-PET/CT.
Materials and Methods
67 consecutive patients (38 male, 29 female; mean age 73 years) with 71 nodules underwent dynamic CE-perfusion ADCT and MRI, PET/CT, and microbacterial and/or pathological examinations. 71 nodules were classified into two groups based on the final diagnoses: malignant (n=45) and benign nodules (n=26). All dynamic CE-perfusion ADCT examinations were performed on a 320-detector row CT (Aquilion ONE, Toshiba Medical Systems Corporation, Otawara, Japan), and dynamic CE-perfusion MRI using parallel imaging technique (TR 2.9 ms/ TE 1.1 ms/ flip angle 12 degree, reduction factor 2) at a 3T system (Vantage Titan 3T, Toshiba). All PET/CT examinations were performed by using standard technique on a PET/CT scanner (Discovery 600M, GE Healthcare, Waukesha, Wisc). In each patient, total perfusion and nodule perfusions from pulmonary and systemic circulations were calculated by dual-input maximum slope method from on dynamic ADCT and MRI. Then, all dynamic ADCT and MR indexes as well as SUVmax in each nodule were determined by ROI measurement.
To compare each index between malignant and benign nodules, Student’s t-test was performed. Then, ROC analyses were performed to compare diagnostic performance and determine feasible threshold values of all indexes. Finally, sensitivity, specificity and accuracy were compared each other by using McNemar’s test.
Results
Representative case is shown in Figure 1.
All indexes had significant difference between malignant and benign nodules (p<0.001).
Results of ROC analysis and compared diagnostic capabilities are shown in Figure 2 and 3. Area under the curves (Azs) of total perfusion of dynamic ADCT (Az=0.89) and MRI (Az=0.88) were significantly larger than that of systemic arterial perfusions on both methods (ADCT: Az=0.75, p<0.05; MRI: Az=0.81, p<0.05). When feasible threshold values adopted, accuracies of total perfusion on dynamic ADCT (87.3%) and MRI (87.3%) was significantly higher than that of systemic arterial perfusions (ADCT: 77.5%, p=0.008; MRI: 77.5%, p=0.008) and SUVmax (78.9%, p=0.02).
Conclusion
Quantitatively assessed dynamic first-pass CE-perfusion ADCT and MRI indexes have better potential than PET/CT for differentiating malignant from benign nodules. In addition, both quantitative perfusion methods were considered as having same potential in this setting.Acknowledgements
This work was technically and financially supported by Toshiba Medical Systems, and financially supported by Guerbet Japan and Bayer Pharma.References
1. Ohno Y, Hatabu H, Takenaka D, Adachi S, Kono M, Sugimura K. Radiology. 2002; 224: 503-511.
2. Ohno Y, Koyama H, Takenaka D, et al. J Magn Reson Imaging. 2008; 27: 1284-1295.
3. Cronin P, Dwamena BA, Kelly AM, Carlos RC. Radiology. 2008; 246: 772-782.
4. Ohno Y, Nishio M, Koyama H, et al. Radiology. 2015; 274: 563-575.
Figures
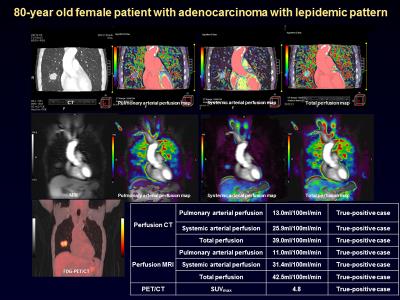
Figure 1. 80-year old female patient with adenocarcinoma with lepidemic pattern (First line from L to R: Thin-section MPR image to pulmonary arterial, systemic arterial and total perfusion maps from dynamic ADCT data, second line from L to R: Source image to pulmonary arterial, systemic arterial and total perfusion maps from dynamic MRI data, and third line: PET/CT and Table of each index in this case).
When applied each feasible threshold value, all indexes could accurately diagnose this nodule as malignant. This case is true positive case in all cases.
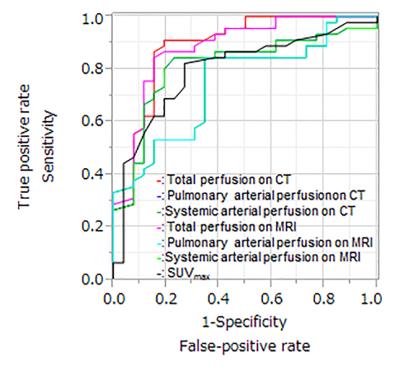
Figure 2. Results of ROC analysis among all indexes.
Area under the curves (Azs) of total perfusion on ADCT (Az=0.89) and MRI (Az=0.88) were significantly larger than that of systemic arterial perfusion ADCT (Az=0.75, p<0.05) and MRI (Az=0.75, p<0.05).
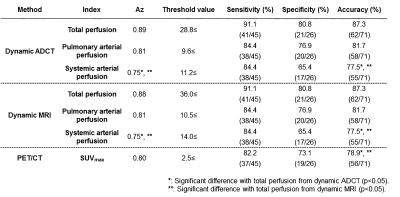
Figure 3. Comparison of diagnosic performance among all indexes.
Azs and/ or accuracy of total perfusions on dynamic ADCT and MRI were significantly higher than those of systemic arterial perfusion on dynamic ADCT and MRI (p<0.05) and SUVmax on PET/CT (p<0.05).