4861
Evaluation of renal oxygenation change by functional MRI with administration of furosemide in diabetic nephropathy modelRui Wang1, Zhiyong Lin1, and Xueqing Sui1
1Radiology, Peking University First Hospital, Beijing, People's Republic of China
Synopsis
Our study was to assess renal hemodynamics and oxygenation using blood oxygen level dependent (BOLD) and oxygen extraction fraction (OEF) imaging in diabetic nephropathy (DN) rabbits following administration of furosemide.
Purpose
To assess renal hemodynamics and oxygenation using blood oxygen level dependent (BOLD) and oxygen extraction fraction (OEF) imaging in diabetic nephropathy (DN) rabbits following administration of furosemide.Methods
Seventeen New Zealand rabbits were randomized into 2 groups: DN group (intravenous injection of alloxan at 100 mg/kg, n = 12); and control group (injection with the same dosage of 0.9% saline, n = 5). Rabbits with blood glucose level >16.0 mmol/L at 3 days after injection were considered as successfully established of diabetes mellitus (DM) model. MR examination was performed using a 3T scanner with an 8-channel knee coil. For each rabbit, MR exam was repeated 4 times: baseline; injection of furosemide (6 mg/kg) immediately after baseline scan, 5 min after furosemide injection; 3 days after modeling (Day 3); 5 min after furosemide injection. BOLD imaging was conducted with multiple-echo spoiled gradient recalled echo (SPGR) sequence by prescribing with 12 echoes (TEs). OEF imaging was derived from Yoblonsky’s model based on multi-echo gradient and spin echo sequence. After scanning, the rabbits were sacrificed for pathological examination. Quantitative RBF, R2* and OEF values were obtained within manually drawn ROIs, including cortex (CO), outer stripes (OS) and inner stripes (IS) of the outer medulla. Independent-sample and paired-sample T test were used to test the differences of R2* and OEF for inter- and inner-group, respectively.Results
Ten of 12 rabbits in the DN group were successfully established. As shown in Figure 1, swelling and mild vacuolation of renal tubular cell and lymphocytes infiltration were observed in DN group. There was no statistically significant difference of R2* or OEF between the two groups at baseline (all p>0.05). Compared with baseline, R2* and OEF in CO, OS and IS at Day 3 were significantly increased in DN group (R2*, baseline vs Day 3: 25.36±6.97 vs 39.95±8.41Hz for CO, p=0.03; 38.24±6.11 vs 55.07±8.57 Hz for OS, p=0.01; 29.11±3.53 vs 54.20±8.91 Hz for IS, p=0.004; OEF, baseline vs Day 3: 0.37±0.05 vs 0.53±0.05 for CO, p=0.004; 0.45±0.05 vs 0.58±0.06 for OS, p=0.02; 0.42±0.01 vs 0.58±0.05 for IS, p=0.003), while no significant change was found in the control group. At baseline, significant decreases of R2* and OEF in OS and IS were observed after furosemide both in control group (baseline, Pre- vs Post-furosemide: 34.66±3.45 vs 23.33±2.07 Hz for R2* in OS, p=0.02; 38.42±6.92 vs 25.00±4.82 Hz for R2* in IS, p=0.04; 0.49±0.03 vs 0.45±0.02 for OEF in OS, p=0.008; 0.44±0.03 vs 0.39±0.03 for OEF in IS, p=0.04) and DN group (baseline, Pre- vs Post-furosemide: 38.24±6.11 vs 27.62±5.09 Hz for R2* in OS, p=0.01; 29.11±1.82 vs 18.66±1.21 Hz for R2* in IS, p=0.03; 0.45±0.06 vs 0.36±0.09 for OEF in OS, p=0.03; 0.42±0.01 vs 0.34±0.01 for OEF in IS, p=0.003). But at Day 3, the corresponded values in DN group were only slightly decreased without statistical significance after furosemide injection (Day 3, Pre- vs Post-furosemide: 55.07±8.57 vs 54.85±8.01Hz for R2* in OS, p=0.97; 54.20±8.91 vs 50.6±9.15 Hz for R* in IS, p=0.43; 0.58±0.06 vs 0.56±0.06 for OEF in OS, p=0.54; 0.58±0.05 vs 0.52±0.06 for OEF for IS, p=0.16).Discussion
This study showed the feasible of accessing renal oxygenation in DN rabbits based on BOLD and OEF imaging. Based on the proposed method, blood R2* and OEF were obtained simultaneously. Our study showed that the region with increased R2* values was corresponding to the region with decreased oxygenation in kidneys of the DM group on Day 3. After furosemide injection, significantly decrease of R2* and OEF in medulla (OS and IS) in control group was observed, while in DM group at Day 3 no significance was found. This indicated that the regulatory function of renal medulla was impaired. If we apply BOLD and OEF in diabetes, it would be valuable for clinicians to detect early renal blood oxygen changes. Also, we hope that BOLD and OEF imaging combined with other technique such as arterial spin labeling (ASL) and DWI imaging could provide complementary assessment of renal pathophysiological changes in a single examination.Acknowledgements
No acknowledgement found.References
No reference found.Figures
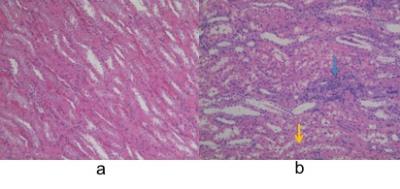
Figure 1: Histologic
examination of renal tissues in controls (a) versus diabetes mellitus (DM) group (b). (Hematoxylin-eosin
stain; original magnification, × 100.) Swelling and mild vacuolation of renal
tubular cell (yellow arrow) and lymphocytes infiltration (blue arrow) were observed in figure 1b.

Figure 2: RBF, R2* and OEF values of pre-furosemide and post-furosemide in CO, OS, IS of DN group. FSM: furosemide. *: p<0.05
At baseline, significant decreases of R2* and OEF in OS and IS were observed after furosemide at baseline in DN group. However, at Day 3, the corresponded values in DN group were only slightly decreased without statistical significance after furosemide injection.