4855
Oxygen Extraction Fraction imaging of kidney after administration of 2 types of iodinated contrast medium: a time course study in CIN animal modelsKai Zhao1, Xueqing Sui1, Rui Wang1, Zhiyong Lin1, Xiaodong Zhang1, Jian Luo1, and Xiaoying Wang1
1Department of Radiology, Peking University First Hospital, Beijing, People's Republic of China
Synopsis
MEGSE imaging is a preeminent noninvasive method to quantify renal oxygen extraction fraction, which may be helpful to understand the pathogenesis of CIN. Our time course study indicates that the iodinated contrast medium can inrease the OEF in different zones of kidney. And some differences do exist on the renal Oxygen Extraction Fraction (OEF) after the two kinds of iodinated CM administration.
Introduction and Purpose
Usage of iodinated contrast medium (CM) during radiological procedure may cause contrast induced nephropathy (CIN), which has drawn an increasing attention in the whole world. The purpose of this study is to find out the chronological effect of 2 types of iodinated contrast medium in Oxygen Extraction Fraction (OEF) by Multi Echo Gradient and Spin Echo (MEGSE) imaging in CIN animal models.Method
Seventeen New Zealand white rabbits were divided into 3 groups: Group A (Iodixanol-270, n=6), Group B (Iohexol-350, n=6), Group C (0.9% saline, n=5). Respiratory anesthesia was used. MR studies were conducted in a 3.0T GE MR scanner with a knee coil. OEF was derived from Yablonsky’s model with MEGSE sequence. A sequential MEGSE sequence was performed to estimate the OEF at 24h before and 5min, 24h, 48h, 72h after contrast or saline administration. Iodinated contrast agent with a dose of 1380 mg I/kg were injected to the experimental groups (Group A and B), and 0.9% saline with a dose of 5.1 ml/kg (to keep the liquid load equal) was administrated to the control group (Group C). OEF values obtained in the cortex (CO), outer stripe of the outer medulla (OS), inner stripe of the outer medulla (IS) were grouped into 5 time-points : “baseline”, “5min”, “24h”, “48h”, “72h” respectively. Then at last the pathology was obtained. Paired sample t-test was performed to test the change of OEF after iodine administration within each group, and One-Way ANOVA was performed to test the response among the 3 groups in each time-point.Results
The iopamidol induced decrease in OEF in the CO, OS or IS of the kidney compared with the saline, which was shown in Table 1, 2, 3 and Figure 1. Among the 3 groups, there was no significant difference in the CO, OS and IS before administration. Iohexol-350 produced higher OEF in the CO, OS and IS while Iodixanol-270 induced higher OEF only in the IS. As for pathology, significant differences were detected after large dose iopamidol administration in the iodine group (Figure 2, 3, 4). Iopamidol produced moderate to severe tubular epithelial cellular swelling, vacuolar degeneration, necrosis and shedding into the tubular lumens. Focal or multifocal lymphocytes and mononuclear cells infiltration in the interstitium appeared in most of the kidneys. The pathologic changes in Group B was more serious than that in Group A. For the kidneys in the saline group (Group C), light microscopic examinations showed that there was no obvious pathological change in the glomeruli.Discussion
In this study, rabbits with CIN are animal models. Usage of iodinated contrast medium during radiological procedure may cause CIN. In human, CIN is characterized by an increase in the serum creatinine (Scr) level of at least 0.5 mg/dl or 25% compared to baseline values in the absence of an alternative etiology1. CIN is more and more significant with the increasing use of enhanced CT and interventional diagnosis and treatment. MEGSE imaging is a preeminent noninvasive method to quantify renal oxygen extraction fraction, which may be helpful to understand the pathogenesis of CIN. Our time course study indicates that the iodinated contrast medium can inrease the OEF in different zones of kidney. And some differences do exist on the renal Oxygen Extraction Fraction (OEF) after the two kinds of iodinated CM administration.The effect produced by Iohexol-350 is more extensive that by Iodixanol-270. The pathology results also confirmed the result. The pathologic changes in Group B was more serious than that in Group A. As we know, the osmotic pressure of Iodixanol-270 (290 mOsm/kgH2O) is much lower than that of Iohexol-350 (844 mOsm/kgH2O). At the same time, the viscosity of Iodixanol-270 (11.3 mPa·s) is also lower than that of Iohexol-350 (11.6 mPa·s). Which factor is the most important? Osmotic pressure? Viscosity? Or other innner factors of CM? More research is needed to figure out which kind of contrast medium is less harmful to human.Conclusion
The increase of renal oxygen extraction fraction produced by Iohexol-350 is more extensive that by Iodixanol-270, which can be detected by MR MEGSE imaging and be confirmed by pathology.Acknowledgements
No acknowledgement found.References
1. Thomsen HS. Guidelines for contrast media from the European Society of Urogenital Radiology. AJR American journal of roentgenology. 2003;181(6):1463-1471.Figures
Tables
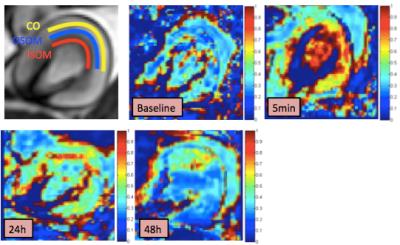
Figure 1: Kidney partition and a
time-course changes of OEF in one rabbit of Group B.

Figure 2: Gross
pathology. The The boundary between cortex and medulla was obscure in Group A
and B (A). The boundary between cortex and medulla was distinct in Group C (B).
Dark apperence and some bleeding of kidney in iodine group (C,D).
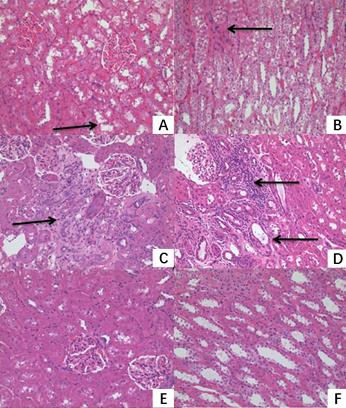
Figure 3: Light microscopic
examinations. Iopamidol produced moderate to severe tubular epithelial cellular
swelling, vacuolar degeneration, necrosis and shedding into the tubular lumens.
Focal or multifocal lymphocytes and mononuclear cells infiltration in the
interstitium appeared in most of the kidneys (A, B, C, D). For the kidneys in
the saline group, light microscopic examinations showed that there was no
obvious pathological change in the glomeruli (E, F).
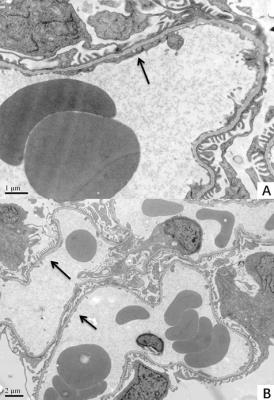
Figure 4: Electron
microscopic examinations. Segmental fusion of the podocyte was seen in both
Group A and B with foot process hole shrink or disappear (A,B)