4843
MRI of Non-obstetric Acute Pelvic Pain in Pregnant Patients1Radiology, Yale New Haven Health Bridgeport Hospital, Bridgeport, CT, United States, 2Yale New Haven Health Bridgeport Hosptial, Bridgeport, CT, United States
Synopsis
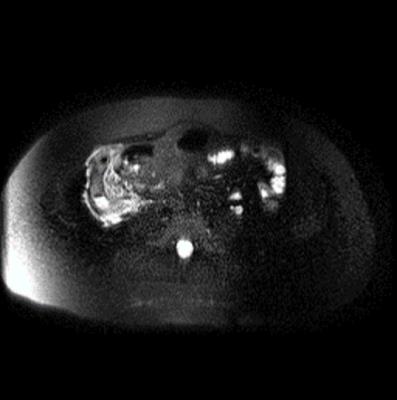
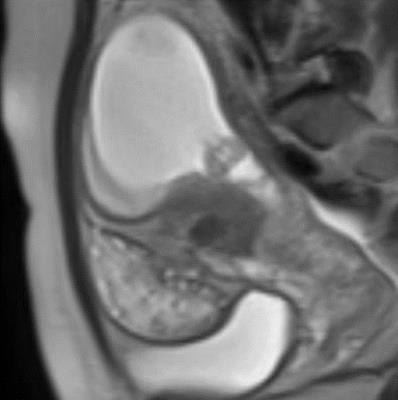
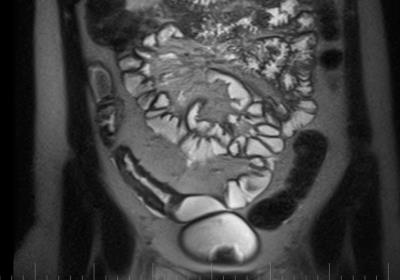
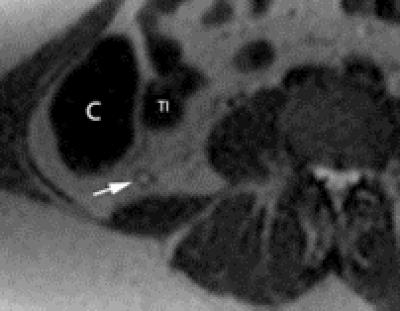
Acute abdominopelvic pain is a common concern during pregnancy. The differential diagnosis for pelvic pain is extensive and includes multiple non-obstetric etiologies. MRI is effective in evaluating pregnant patients with acute abdominopelvic pain.
MRI provides a complete cross-sectional evaluation of the abdomen and pelvis without radiation exposure or the need for intravenous contrast. MRI can help with the diagnosis in pregnant women with acute pelvic pain expediting treatment, especially when ultrasound results are indeterminate. MRI can also prevent unnecessary surgical exploration which carries a high risk to the pregnancy secondary to preterm uterine contractions.
We provide a list and MR imaging examples of differential diagnoses of acute non-obstetric pelvic pain in pregnancy.
Learning Objectives
−The utility of MRI in the evaluation of the pregnant patient with acute abdominopelvic pain is discussed.
−The non-obstetric causes of abdominopelvic pain in a pregnant female are reviewed throughout this presentation.
−MR images are used to illustrate the findings for diagnosis of these pathologies.
Table of Contents
−Background.
−Cases:
Acute Appendicitis.
Ovarian Torsion.
Obstructive Uropathy, Pyelonephritis and Cystitis.
Abscess.
Ovarian Cysts and Cystic Lesions.
Inflammatory Bowel Disease.
Uterine Leiomyomas
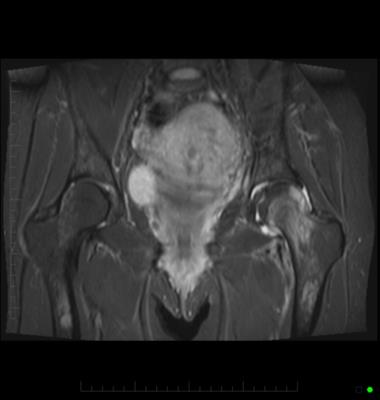
Musculoskeletal: Transient osteoporosis of the hip and Sacroiliitis.
−Conclusion.
Background
Acute abdominopelvic pain is a common concern in pregnant patients. Multiple nonobstetric etiologies are included in the differential diagnoses of abdominopelvic pain in pregnancy. During pregnancy, clinical history, physical exam and laboratory findings are frequently nonspecific. For this reason, diagnostic imaging is usually obtained in pregnant women with acute abdominopelvic pain.
Ultrasound is a safe, inexpensive imaging modality and is the first imaging modality of choice in pregnant patients. However, ultrasound is operator dependent and can be limited due to body habitus or displacement of the normal anatomy by the gravid uterus. Subsequently, MRI has an increasing role in this setting. MRI is a sensitive and specific imaging modality which provides cross-sectional imaging of the entire abdomen and pelvis without radiation risk to the fetus. MRI provides excellent anatomic detail and soft tissue contrast helping differentiate between pathologies causing acute abdominopelvic pain.
Studies have shown that in pregnant patients with acute abdominopelvic pain, MRI demonstrates 89% sensitivity and 95% specificity for patients requiring surgical treatment. Gadolinium contrast is categorized in the FDA Category C drug during pregnancy, and is not routinely administered as the long term effects of gadolinium exposure in utero are not known. Fortunately, gadolinium contrast is needed to make a diagnosis in many cases given fluid sensitive MR sequences that can identify inflammation and optimal soft tissue contrast. The effects of MRI in the first trimester are not well known and current recommendations recommend avoiding MR imaging during this time unless the benefits outweigh the risks.
Conclusion
MR imaging is effective in evaluating and triaging pregnant women with acute abdominopelvic pain. MRI provides a systematic cross-sectional evaluation of the abdomen and pelvis without radiation exposure or the need for intravenous contrast.
MRI can help with the diagnosis in pregnant women with acute pelvic pain expediting treatment, especially when ultrasound results are indeterminate. MRI can also prevent unnecessary surgical exploration which carries a high risk to the pregnancy secondary to preterm uterine contractions.
MRI during pregnancy does carry the potential for adverse effects due to exposure to high intensity magnetic fields, radiofrequency pulses and excessive noise. However, there have been no adverse events reported to date. Data concerning MRI in the first trimester is limited and extra caution is taken before imaging during this stage of pregnancy. Despite these concerns, MRI is considered a relatively safe modality during pregnancy and has an important role in the evaluation of pregnant women with pelvic pain.
Acknowledgements
No acknowledgement found.References
Lubarsky, M. et al. "MR Imaging for Acute Non-traumatic Abdominopelvic Pain: Rationale and Practical Considerations." Radiographics(2013) 33(2):313-373.
Long, S. et al. "Imaging Strategies for Right Lower Quadrant Pain in Pregnancy." AJR(2011) 196:4-12.
Masselli, G. et al. "Acute Abdominal and Pelvic Pain in Pregnancy: MR Imaging as a Valuable Adjunct to Ultrasound." Abdominal Imaging(2011) 36:596-603.
Oto, A. et al. "MR Imaging in the Triage of Pregnant Patients with Acute Abdominal and Pelvic Pain." Abdominal Imaging(2009) 34:243-250.
Singh, A. et al. "Emergency MRI of Acute Pelvic Pain: MR Protocol with No Oral Contrast." Emergency Radiology(2009) 16:133-141.
Kurzel, R. et al. "Magnetic Resonance Imaging of Peripartum Rupture of the Symphysis Pubis." Obstetrics and Gynecology(1996) 87:826-829.
Parker, J. and M. Bhattacharjee. "Peripartum diastasis of the Symphysis Pubis. New England Journal of Medicine(2009) 361:1886.
Willis-Owen, C. et al. "Bilateral Femoral Neck Fractures Due to Transient Osteoporosis of Pregnancy: A Case Report." Cases Journal(2008) 1:120.
Figures