4828
Amplitude-probability sorting for single-pass, retrospective 4D-MRI using 2D bSSFP MRI with interleaved cylindrical navigators1Radiation Oncology, Mayo Clinic, Rochester, MN, United States, 2GE Healthcare, Waukesha, WI, United States, 3Radiation Oncology, Mayo Clinic, Phoenix, AZ, United States, 4GE Healthcare, New York, NY, United States, 5Radiology, Mayo Clinic, Rochester, MN, United States
Synopsis
With MRI being increasingly incorporated in the radiotherapy workflow, the multidisciplinary community has a strong interest in developing “4D-MRI” techniques for both offline (tumor motion characterization for treatment planning) and online (tumor motion tracking) applications. In a cohort of 10 volunteers, the present study applied 2D (coronal) bSSFP with interleaved cylindrical navigators monitoring the liver dome to retrospectively derive 4D-MRI comparing two sorting methods, namely phase and amplitude-probability. Amplitude-probability binning was shown, both qualitatively and quantitatively, to reduce “volume inconsistencies” caused by variable breathing.
Purpose
The characterization of respiratory motion using MRI, i.e., “4D-MRI,” is an important area of development for radiation therapy treatment planning applications1. Many 4D-MRI methods involving 2D and 3D sequences have been proposed over the last decade, but their translation to routine clinical practice is lacking. 2D approaches using fast dynamic sequences are advantageous in terms of practicality; moreover, they provide a direct analog with the current radiotherapy standard, 4D-CT. However, 4D-MRI reconstructions via 2D MRI are subject to volume-inconsistency artifacts given the prevalence of breathing irregularities. To address this, retrospective reconstruction approaches have been proposed2-4; meanwhile, use of internal (or internal anatomy-based) motion surrogates for derivation of respiratory state provides clear advantages over external surrogates. The purpose of this study was to evaluate whether a hybrid “amplitude-probability” approach based on an internal motion surrogate improves 4D-MRI volume consistency versus standard phase-based sorting.Methods
MRI
Ten normal volunteers consented for an IRB-approved study and were imaged coronally under free breathing conditions on a 3T widebore system (MR750w, GE Healthcare, Waukesha, WI) using a 2D balanced steady-state free precession (bSSFP) sequence including cylindrical navigator echoes interleaved between successive image frames5. Navigators were positioned to monitor the liver dome craniocaudally. To allow for sufficient sampling of 10 reconstructed 4D/respiratory bins, 30 cine images were acquired at each slice location (all dynamics acquired before moving to the next slice location)6,7. The FOV included the lungs/upper-abdomen (3602-4202 mm2 on matrix of 192×192 or 200×200) with a slice profile thickness of 5mm. Repetition time (frame rate) spanning single-shot bSSFP+navigator waveforms varied from 383-493ms with a flip angle of 35°. The first two volunteers’ exam included 17 slices; the remaining eight volunteers’ exams included either 31 or 33 slices.
Retrospective Sorting
Retrospective, single-pass sorting and slice stacking was performed using in-house software (Matlab, The Matworks, Inc., Natick MA) and DICOM 2D images. Navigator profiles (from an acquisition log file) were analyzed to determine the dome/edge position or equivalent mathematical surrogate (Figure 1a). Subsequently, timing information (from an additional log file) was used to interpolate this set of surrogate positions onto a uniform temporal grid synchronized with imaging. (Herein, spline interpolation was employed with 4× temporal upsampling to improve inspiratory peak localization). Respiratory bin values (computed as continuous variables) per time point were determined using two methods – standard phase and amplitude-probability2,8 (Figure 1c). Amplitude-probability binning involved generating dome/surrogate position distributions for inhalation and exhalation and asserting that each bin spans an equal-area portion of said distribution (hence equal-probability) (Figure 1b). DICOM tag TriggerTime was referenced to assign a continuous phase and amplitude-probability bin value per 2D image. 2D image selection for phase- and amplitude-probability-4D-MRI was based on continuous bin values being nearest the given central bin value.
Volume Consistency Analyses
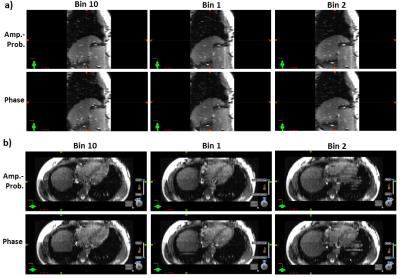
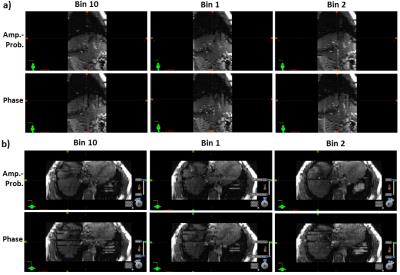
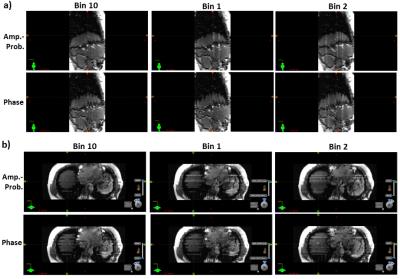
Volume consistency of phase- versus amplitude-probability-4D-MRI was assessed both qualitatively and quantitatively. Qualitative inspection was carried out via visual comparison of side-by-side sagittal and axial 3D cut-planes at the liver dome position for the three bins closest to peak inhalation (10,1,2). Quantitative analyses incorporated 11 contiguous sagittal cut-planes: within a 2D ROI that encompassed the liver dome and was common over all slices and bins for a given volunteer, the anterior-posterior (x) directional image (≡I) gradient magnitude image (≡|dI/dx|) was calculated using Matlab function imgradientxy (Figure 2a). A mean anterior-posterior image gradient magnitude (≡mean|dI/dx|) was derived by averaging over all pixels and over 11 slices; this calculation was tallied for each respiratory bin. To remove the signal bias introduced by motion of anatomy relative to fixed 2D ROI selection, mean|dI/dx| for phase-based sorting (≡mean|dI/dx|phase) was normalized by the same result for amplitude-probability sorting, per bin.
Results
Significant breathing irregularity, and hence volume inconsistency, was observed in several volunteers. The average value of mean||dI/dx|phase/mean||dI/dx|amp.-prob. over all volunteers and respiratory bins was 1.0325 (95% C.I. [1.0089-1.0562]), indicating a statistically-significant improvement in volume consistency (of the liver dome) for amplitude-probability-based binning (Figure 2b). Qualitative inspection was convincingly in favor of amplitude-probability binning (Figures 3-5).Discussion
The image gradient metric used here will likely be applied for future studies of retrospective 4D-MRI derived using the current sequence versus using 2D single-shot fast spin echo with an interleaved phase acquisition order (GE Healthcare)5. This would serve as in vivo verification of a previous in silico study7.Conclusion
We have established amplitude-probability as an improvement over standard phase-based sorting for (either single-pass or iterative) retrospective sorting in a cine acquisition mode. This has direct relevance for ongoing work focused around clinical translation.Acknowledgements
No acknowledgement found.References
1. McGee KP, Hu Y, Tryggestad E, Brinkmann D, Witte B, Welker K, Panda A, Haddock M, Bernstein MA. MRI in radiation oncology: Underserved needs. Magn Reson Med. 2016; 75(1): 11-4.
2. Tryggestad E, Flammang A, Han-Oh S, Hales R, Herman J, McNutt T, Roland T, Shea SM, Wong J. Respiration-based sorting of dynamic MRI to derive representative 4D-MRI for radiotherapy planning. Med Phys. 2013; 40(5): 051909.
3. R Farah, S Shea, E Tryggestad, R Teboh Forbang, J Wong, R Hales, J Lee. 4D-MRI Reconstruction Using Group-Wise Registration. Med. Phys. 2015. 42: 3537.
4. von Siebenthal M, Székely G, Gamper U, Boesiger P, Lomax A, Cattin P. 4D MR imaging of respiratory organ motion and its variability. Phys Med Biol. 2007; 52(6): 1547-64.
5. Litwiller DV, Tryggestad E, McGee K, Iwadate Y, Estkowski L, Bayram E. Single-Shot, Navigator-Based Approach to Retrospective 4D MRI: balanced-SSFP vs. Single-Shot Fast Spin Echo. ISMRM 24th Annual Meeting and Exhibition, May 7-13, 2016, Singapore.
6. Liu Y, Yin FF, Chen NK, Chu ML, Cai J. Four dimensional magnetic resonance imaging with retrospective k-space reordering: a feasibility study. Med Phys. 2015; 42(2):534-41.
7. Liu Y, Yin FF, Rhee D, Cai J. Accuracy of respiratory motion measurement of 4D-MRI: A comparison between cine and sequential acquisition. Med Phys. 2016; 43(1): 179.
8. Olsen JR, Lu W, Hubenschmidt JP, Nystrom MM, Klahr P, Bradley JD, Low DA, Parikh PJ. Effect of novel amplitude/phase binning algorithm on commercial four-dimensional computed tomography quality. Int J Radiat Oncol Biol Phys. 2008; 70(1): 243-52.
Figures