4824
Comparing the invasive depth of esophageal carcinoma in 3.0 T ex vivo T2-mapping MR imaging with histopathological findings1MR Research China, GE Healthcare, Beijing, People's Republic of China, 2Radiology, Zhengzhou University People's Hospital, Zhengzhou, People's Republic of China
Synopsis
Esophageal carcinoma is the eighth most common cancer worldwide with a rising incidence. It has been demonstrated that the normal esophageal wall can be depicted as eight layers in T2 weighted MRI , however only qualitative assessment has been made so far. In this work, an ex vivo experiment was conducted on 3.0T clinical scanner to prospectively establish the quantitative T2 value as a means of depicting the normal esophageal wall by T2-mapping and evaluate the depth of the carcinoma invasion using histopathological as a reference.
Purpose
Esophageal carcinoma is the eighth most common cancer worldwide with a rising incidence [1]. However, the overall prognosis of esophageal carcinoma remains poor because the initial diagnoses are only feasible at later stages. Computed tomography (CT) could not depict the specific layer invasion of the esophageal wall due to its poor soft-tissue contrast. Endoscopic ultrasonography (EUS) can be used to depict the esophageal layers but is restricted by high operator dependency, issues that result from the pathologically stenotic esophageal wall, and its semi- invasive nature. It has been demonstrated that the normal esophageal wall can be depicted as eight layers in T2 weighted MRI [2], however only qualitative assessment has been made so far. In this work, the use of quantitative T2-mapping as a means of depicting the normal esophageal wall and evaluating the thickness of the carcinoma using histopathological as a reference is investigated.Methods
This prospective study was approved by the Ethics Committee of our hospital and written informed consents were obtained from all patients. The study population contained 22 esophageal specimens from 22 patients with newly diagnosed esophageal carcinoma by preoperative gastroscopy biopsy . The length of esophageal specimens ranged from 70 to 222 mm (146±76mm, mean±std). For all examinations, studies were carried out on a 3.0-T MR system (Discovery MR750, GE Healthcare, Milwaukee, USA). A four-channel phased-array 3.5 inches animal coil was used for all measurements. A spin echo based T2-mapping acquisition was made: TR/TE = 1518/10.4ms; slice thickness = 3.0 mm; FOV = 60×36 mm2; matrix = 256×192 and NEX= 1. A freehand ROI was placed to measure T2 value of the normal esophageal layers and carcinoma. Three independent readers who were blindly to the histopathological findings measured the depth of the carcinoma invasion. The removed esophageal specimens were fixed with formalin and stained with hematoxylin-eosin (H-E). The specimens were sectioned transversely with a 5-um-slices, a pathologist measured the depth of the carcinoma invasion on the largest transverse diameter of the tumor. The MR images of tumors’ invasive depth were compared with the histopathological findings as the standard reference. Games-Howell test was used to compare the difference between the normal esophageal layers and carcinoma. Bland-Altman scatter plots were used to measure the consistency between the inter- and intra-observer agreement.Results
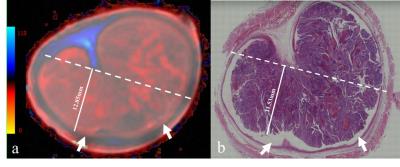
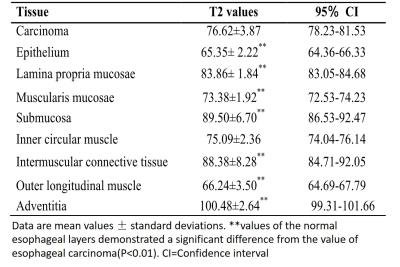
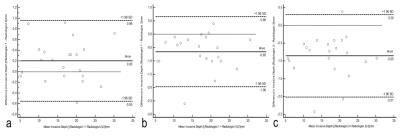
T2-mapping MR images can be used to clearly depict the eight normal esophageal layers and the carcinoma (Figure 1). The T2 value between the carcinoma and normal esophageal layers demonstrated a statistical significance (all P<0.01), except for the inner circular muscle (P=0.808) (Table 1). Bland-Altman scatterplots demonstrated that the discrepancy of the depth of the carcinoma invasion among the three radiologists and the histopathological analysis were 1.3 mm、1.2 mm and 1.3 mm (Figure 2), the mean discrepancy for the inter-observer were 0.06 mm、0.05 mm and 0.13 mm (Figure 3), which demonstrated good consistency.Discussion and Conclusion
Acknowledgements
No acknowledgement found.References
[1] Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet (London, England) 2013;381(9864):400-412.
[2] Wei Y, Wu S, Shi D, et al. Oesophageal carcinoma: comparison of ex vivo high-resolution 3.0 T MR imaging with histopathological findings. Sci Rep. 2016 Oct 11; 6:35109.
[3] Glaser C. New techniques for cartilage imaging: T2 relaxation time and diffusion-weighted MR imaging. Radiol Clin North Am. 2005;43(4):641-53
Figures