4813
Myometrial invasion in endometrial cancer: Comparison of reduced field-of-view diffusion-weighted imaging and dynamic contrast-enhanced magnetic resonance imagingMayumi Takeuchi1, Kenji Matsuzaki2, and Masafumi Harada1
1Department of Radiology, Tokushima University, Tokushima, Japan, 2Department of Radiological Technology, Tokushima Bunri University, Sanuki-city, Japan
Synopsis
The depth of myometrial invasion was evaluated in 25 patients with surgically proven endometrial cancer by T2WI, reduced field-of-view DWI (rFOV-DWI) and 3D dynamic contrast-enhanced MRI (DCE-MRI). The depth of myometrial invasion (stage S: <50% vs stage D: ≥50%) on MRI was correlated with surgical pathology results. The staging accuracy was 68% for T2WI, 92% for DCE-MRI, and 96% for rFOV-DWI. Combination of rFOV-DWI reading together with T2WI improved the assessment of myometrial invasion with a diagnostic accuracy of up to 100%. Especially, rFOV-DWI has an advantage in assessing the depth of myometrial invasion in cases with coexisting adenomyosis.
Background and purpose of the study
The assessment of depth of myometrial invasion is important in evaluating endometrial cancer on MRI, because it closely correlates with the prevalence of nodal metastasis and the patient’s prognosis. DWI demonstrates endometrial cancer as a high signal intensity mass, however, detailed evaluation of myometrial invasion on conventional DWI is occasionally difficult due to low spatial resolution and distortion1-3. Reduced phase direction field-of-view (FOV) technique by using spatially selective phase encoding gradient can offer high quality DWI with improved spatial resolution, without associated phase wrap round artifact, and with less artifacts related to motion and susceptibility which are common in larger FOV images4, 5. The purpose of this study is to compare the diagnostic performance of reduced FOV DWI (rFOV-DWI) with those of T2WI and 3D dynamic contrast-enhanced MRI (DCE-MRI) in evaluating the depth of myometrial invasion.Materials and methods
25 women with endometrial cancer underwent preoperative MRI including T2WI, conventional DWI and rFOV-DWI (b = 0 and 800 sec/mm2) and 3D-DCE-MRI with 3T MRI units (Discovery MR750, GE Healthcare). The depth of myometrial invasion was evaluated on T2WI, rFOV-DWI (FOCUS: FOV optimized and constrained undistorted single shot, FOV:20-24*8-12cm, Matrix:160*80, thickness:5mm), and 3D-DCE-MRI (3D fast spoiled gradient-recalled echo sequence with fat-suppression; FOV:30cm, Matrix:320*192, thickness:3 mm/1.5 mm overlap; with intravenous administration of 0.1 mmol/kg of gadopentetate dimeglumine). The depth of myometrial invasion evaluated on both sagittal and oblique axial (short axis) images by two radiologists was classified as stage S (superficial invasion: limited in the endometrium or invades less than 50% of the myometrium) and stage D (deep invasion: invades 50% or more of the myometrium). The results were compared with the histologically confirmed depth of myometrial invasion to determine the diagnostic accuracy of T2WI, rFOV-DWI and 3D-DCE-MRI, respectively.Results
The 25 surgically proven endometrial cancers included 16 stage S and 9 stage D tumors (Table 1). All 25 tumors exhibited high intensity on rFOV-DWI with clear margins (Fig. 1-4). The depth of myometrial invasion was not able to estimate on T2WI in 8 stage D tumors due to poor tumor-to-myometrium contrast (tumor and adjacent myometrium showed similar signal intensity) (Fig. 2), or due to poor tumor-to-coexisting adenomyosis contrast (Fig. 3), and also not able to estimate on 3D-DCE-MRI in 2 stage D tumors due to poor tumor-to-coexisting adenomyosis contrast (Fig. 3). The myometrial invasion was not able to estimate on rFOV-DWI in one stage S tumor due to distortion caused by susceptibility artifact from adjacent rectal gas (Fig. 4). The staging accuracy was 68% (17/25) for T2WI, 92% (23/25) for 3D-DCE-MRI, and 96% (24/25) for rFOV-DWI. Combination of rFOV-DWI reading together with T2WI improved the assessment of myometrial invasion with a diagnostic accuracy of up to 100%.Discussions
The depth of myometrial invasion strongly correlates with the risk of lymph node metastasis (3% with superficial myometrial invasion and 46% with deep myometrial invasion) and prognosis of the patients with endometrial cancer. Beddy et al. reported that DWI had a higher diagnostic accuracy in assessing the depth of myometrial invasion than did DCE-MRI1. DWI has a high diagnostic accuracy in detecting deep myometrial invasion, and there is no significant difference between sensitivity and specificity of DWI and DCE-MRI according to a meta-analysis3. However, detailed evaluation of myometrial invasion on conventional DWI is occasionally difficult due to low spatial resolution and distortion caused by susceptibility artifacts4, 5. In this study all 25 tumors were demonstrated as high signal intensity masses with clear margins on rFOV-DWI. The depth of myometrial invasion was correctly diagnosed due to good tumor-to-myometrium contrast except for one lesion with distortion caused by susceptibility artifact from adjacent rectal gas. By referring T2WI, the depth of myometrial invasion was correctly assessed in this patient. The depth of myometrial invasion could not be evaluated both on T2WI and on DCE-MRI in 2 patients with coexisting adenomyosis. Adenomyosis may show heterogeneous signal intensity on T2WI and/or heterogeneous contrast enhancement on DCE-MRI, and the boundaries between the tumor and adenomyosis may be unclear2. Our results suggest that rFOV-DWI is helpful for differentiating coexisting adenomyosis and tumor invasion in such cases.Conclusions
We conclude that addition of rFOV-DWI may improve the staging accuracy of endometrial cancer in assessing the depth of myometrial invasion. Especially rFOV-DWI has an advantage in assessing the depth of myometrial invasion in cases with coexisting adenomyosis. rFOV-DWI can be an alternative to DCE-MRI in evaluating myometrial invasion of endometrial cancer without the use of contrast medium.Acknowledgements
No acknowledgement found.References
1) Beddy P, Moyle P, Kataoka M, et al. Evaluation of depth of myometrial invasion and overall staging in endometrial cancer: comparison of diffusion-weighted and dynamic contrast-enhanced MR imaging. Radiology. 2012;262:530-537. 2) Takeuchi M, Matsuzaki K, Nishitani H. Diffusion-weighted magnetic resonance imaging of endometrial cancer: differentiation from benign endometrial lesions and preoperative assessment of myometrial invasion. Acta Radiol. 2009;50:947-953. 3) Andreano A, Rechichi G, Rebora P, et al. MR diffusion imaging for preoperative staging of myometrial invasion in patients with endometrial cancer: a systematic review and meta-analysis. Eur Radiol. 2014;24:1327-1338. 4) Saritas EU, Cunningham CH, Lee JH, et al. DWI of the spinal cord with reduced FOV single-shot EPI. Magn Reson Med. 2008;60:468-473. 5) Thierfelder KM, Scherr MK, Notohamiprodjo M, et al. Diffusion-weighted MRI of the prostate: advantages of Zoomed EPI with parallel-transmit-accelerated 2D-selective excitation imaging. Eur Radiol. 2014;24:3233-3241.Figures
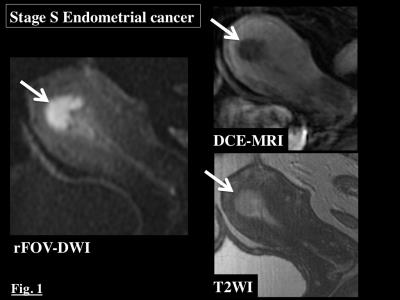
Stage S Endometrial cancer: Endometrial cancer (arrow) is confined within the
endometrium (stage S). Tumor-to-endometrium contrast is good on rFOV-DWI,
whereas that is poor on T2WI and DCE-MRI.
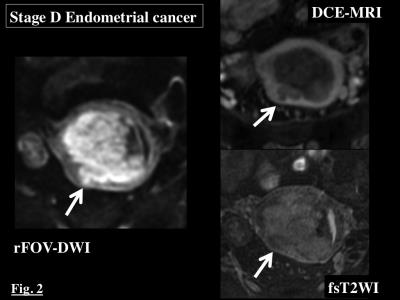
Stage D Endometrial cancer: Endometrial cancer (arrow) invades deeply into the
myometrium (stage D). Tumor-to-myometrium contrast is good on rFOV-DWI and DCE-MRI,
whereas that is poor on T2WI.
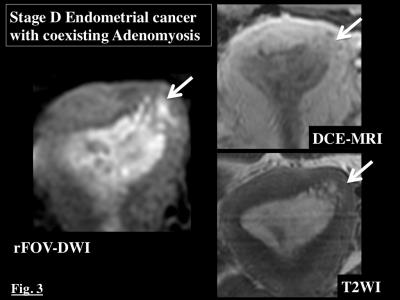
Stage D Endometrial cancer with coexisting
adenomyosis:
Endometrial cancer (arrow) invades beyond the coexisting adenomyosis and into
the deep myometrium (stage D). Tumor extent is clearly visualized on rFOV-DWI
and unclear on T2WI and DCE-MRI.
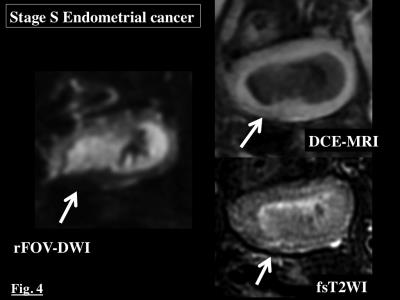
Stage S Endometrial cancer: The boundary between the tumor and the myometrium (arrow)
is clear without myometrial invasion on T2WI and DCE-MRI. Assessment of the
depth of myometrial invasion is not possible due to distortion (arrow) caused
by susceptibility artifact from adjacent rectal gas on rFOV-DWI.
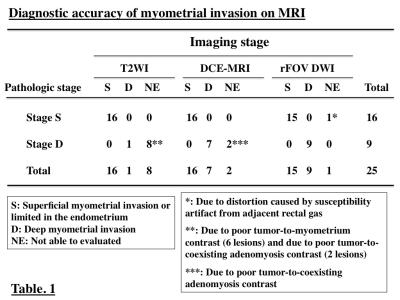
Diagnostic accuracy of myometrial invasion on MRI: MRI staging on T2WI, DCE-MRI, and rFOV-DWI is
shown. The staging accuracy was 68% for T2WI, 92% for DCE-MRI, and 96% for rFOV-DWI.