4810
Safety of 3T MRI Scan for pregnant women: Effect of Maternal Size, Maternal Position and Twin Pregnancy1Fetal-Neonatal Neuroimaging & Developmental Science Center, Boston Children's Hospital, Boston, MA, United States, 2Department of Electrical Engineering and Computer Science, Massachusetts Institute of Technology, Cambridge, MA, United States, 3Harvard Medical School, Boston, MA, United States, 4A. A. Martinos Center for Biomedical Imaging, Department of Radiology, Massachusetts General Hospital, Charlestown, MA, United States, 5Harvard-MIT Health Sciences and Technology, Massachusetts Institute of Technology, Cambridge, MA, United States
Synopsis
Possible temperature increase due to RF exposure during MRI scan of pregnant women can be critical for the fetus. In this study, we perform electromagnetic and temperature simulations using different pregnant women models with different postures. We assess the variability of in-utero RF induced heating in a 3T birdcage coil for different models generated by segmenting structural MR images.
Purpose
Recently, 3T MRI has started to be used in cases where pregnant patient scans are required. To investigate the safety concern related to the RF exposure to the fetus under this setting, several numerical studies were done on pregnant body models at different gestational ages (GA).1-6 Unfortunately, all of these studies were conducted on the same reference body model. In this study we argue that further analysis should be performed to investigate the effect of maternal size and maternal position for better safety management. To this end, we assess the local SAR exposures and the induced temperature increase under 3T for various pregnant body models with different postures.Method
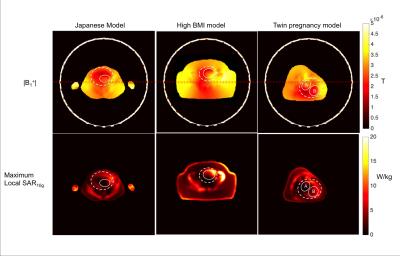
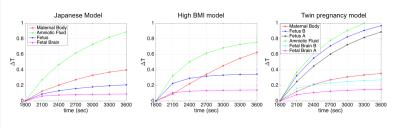
For this study, we obtained consents from two pregnant subjects, i.e. one high body mass index (BMI~45) subject at 28wks+2days GA, and another with monochromic twin pregnancy at 27wks+6days GA, to generate the models. As a third case, the whole-body pregnant model7 (26wks GA) developed by the National Institute of Information and Communications Technology, Tokyo, and Chiba University was used. This model was previously simulated by Hand et al.5 and in this study used as a simulation reference. Model generation: MRIs were performed on a 3T Skyra scanner (Siemens Healthcare, Erlangen, Germany) using a combined 18-channel body matrix and 12-channel spine-receive arrays. Two sets of axial HASTE images (resolution: 2.6x2.6x3 mm3, TR: 1600 ms, TE: 117 ms) with 124 slices each were acquired. 3D abdominal images were manually segmented to identify different organs in 3D Slicer8 and then segmented organs were interpolated to 2x2x2 mm3 resolution. After interpolation, 3 pixel width smoothing was applied to each segmented organ. Further motion artifacts at the organ boundaries were smoothened manually. High BMI and twin pregnancy models included 24 and 30 tissues (i.e. maternal abdominal organs, muscle, fat, skin, bone, aorta, vena cava, uterus, amniotic fluid, umbilical cord, fetus and fetal brain), respectively. Electromagnetic & temperature simulations: Simulations were performed in Sim4Life Version 3.0.1 (ZMT, Zurich, Switzerland). Each body model was placed into a model of two-port, 32 rungs Siemens Skyra birdcage coil and simulated using the circularly polarized mode (CP) excitation. Segmented models were converted to voxel models and together with the tissue descriptor file imported into Sim4Life. Figure 1 demonstrates the position of different models within the coil such that the back (the side for left lateral case) of the models were always placed 20 cm away from the inner edge of the coil. In order to compare the models, exposure configurations were normalized to the normal operating mode, which is 2W/kg whole body average SAR (wbaSAR). By assuming the main energy loss would be within the truncated region, whole body weights were used for the normalization for the segmented models. To validate this assumption, one of the truncated models was extended with additional segments and simulated to reveal that only 2.1% of the total energy loss was measured at the extended regions. For temperature simulations, previously suggested perfusion parameters5 were used by assuming constant perfusion. External air temperature was set as 25°C, while the initial temperatures were 37°C and 37.5°C for maternal and fetal tissues, respectively.5 Temperature change was measured during 3600s where first 1800s was without exposure and second 1800s was with the maximum allowed exposure at 2W/kg wbaSAR.Results and Discussion
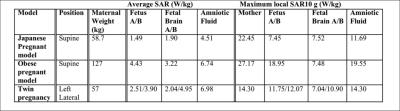
As summarized in Table 1, for both high BMI case and the left lateral positioning when the fetuses were closer to the coil, higher SAR values were observed. More specifically, for twin pregnancy model, higher SAR was measured for the twin closer to the coil. The maximum local SAR was observed in the arm of the Japanese model. Although the arms were not included to the other models, the highest maternal maximum local SAR was observed in the high BMI model. Positioning of the fetuses were demonstrated within |B1+| and local SAR maps in Figure 2. Average temperature changes along the 1800s 2W/kg exposure were shown in Figure 3. It is observed that for high BMI and twin pregnancy models temperature increase faster. Note that, further analysis should be performed by changing the maternal position in the xy-plane and more realistic temperature models should be developed considering the thermoregulation models and the perfusion changes within the uterus due to placental insufficiency or fetal-maternal abnormalities.6,9Conclusion
In this study, we demonstrated that local SAR and temperature increase could change with different maternal size, fetal and maternal positions. We emphasize that to better understand MR safety during pregnancy, it is necessary to perform analysis for different patient models.Acknowledgements
We would like to thank Yigitcan Eryaman, PhD. This project is supported by NIH U01 HD087211 and NIH R01 EB017337.References
1. Hand JW, Li Y, Thomas EL, Rutherford MA, Hajnal JV. Prediction of specific absorption rate in mother and fetus associated with MRI examinations during pregnancy. Magnetic resonance in medicine. 2006 Apr 1;55(4):883-93.
2. Pediaditis M, Leitgeb N, Cech R. RF-EMF exposure of fetus and mother during magnetic resonance imaging. Physics in medicine and biology. 2008 Nov 26;53(24):7187.
3. Nagaoka T, Saito K, Takahashi M, Ito K, Watanabe S. Anatomically realistic reference models of pregnant women for gestation ages of 13, 18, and 26 weeks. 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society 2008 Aug 20 (pp. 2817-2820).
4. Shamsi S, Chen J, Liu R, Kainz W. SAR evaluation of pregnant woman models in 64 MHz MRI birdcage coil. IEEE MTT-S International Microwave Symposium Digest 2006 Jun 11 (pp. 225-228).
5. Hand JW, Li Y, Hajnal JV. Numerical study of RF exposure and the resulting temperature rise in the foetus during a magnetic resonance procedure. Physics in medicine and biology. 2010 Jan 20;55(4):913.
6. Murbach M, Neufeld E, Samaras T, Córcoles J, Robb FJ, Kainz W, Kuster N. Pregnant women models analyzed for RF exposure and temperature increase in 3T RF shimmed birdcages. Magnetic resonance in medicine. 2016 May 1.
7. Nagaoka T, Togashi T, Saito K, Takahashi M, Ito K, Watanabe S. An anatomically realistic whole-body pregnant-woman model and specific absorption rates for pregnant-woman exposure to electromagnetic plane waves from 10 MHz to 2 GHz. Physics in medicine and biology. 2007 Oct 30;52(22):6731.
8. Fedorov A., Beichel R., Kalpathy-Cramer J., Finet J., Fillion-Robin J-C., Pujol S., Bauer C., Jennings D., Fennessy F., Sonka M., Buatti J., Aylward S.R., Miller J.V., Pieper S., Kikinis R. 3D Slicer as an Image Computing Platform for the Quantitative Imaging Network. Magnetic Resonance Imaging. 2012 Nov;30(9):1323-41. PMID: 22770690.
9. Gowland PA, De Wilde J. Temperature increase in the fetus due to radio frequency exposure during magnetic resonance scanning. Physics in medicine and biology. 2008 Oct 8;53(21):L15.
Figures