4804
Comparison of 18F-FDG PET/MRI and MRI alone for pretherapeutic tumor staging of patients with primary cancer of the uterine cervix.1Diagnostic and Interventional Radiology, University Hospital Essen, Essen, Germany
Synopsis
This study demonstrates a successful attempt to utilize and evaluate the diagnostic potential of integrated PET/MRI for staging patients with primary cervical cancer. According to the results, 18F-FDG PET data do not seem to provide useful additional information to MRI for the determination of the local extent of the primary tumors. However, the present results show a better performance of simultaneously acquired 18F-FDG PET and MR datasets for the detection of nodal and distant metastases if compared to MRI alone. Therefore, integrated PET/MR imaging may provide valuable information for treatment planning and to predict prognosis.
Introduction
Highly accurate tumor staging of patients with primary cervical cancer is mandatory to provide an efficient and appropriate treatment strategy. For the determination of the local tumor extent, MRI has been shown the most accurate imaging modality due to the high soft-tissue contrast.1 Accordingly, the use of MRI for the evaluation of primary tumors is recommended in the FIGO classification system at an early tumor stage (FIGO ≥ IB2).2 On the other hand, hybrid imaging, in terms of PET/CT, has been shown superior then conventional imaging techniques (e.g. CT, MRI) for the detection of metastatic spread.3,4 The successful implementation of integrated PET/MR scanners into clinical imaging enables the combination of the diagnostic advantages of MRI and PET, for primary tumor evaluation and the identification of lymph node or distant metastases.5 Therefore, we initiated the study to evaluate and compare the diagnostic performance of integrated PET/MRI and MRI alone for dedicated primary tumor staging of cervical cancer patients.
Methods
A total of 47 consecutive patients with histopathologically confirmed primary cervical cancer underwent a whole-body PET/MRI examination on a 3T Biograph mMR scanner prior to pelvic and/or para-aortic lymphadenectomy and the initiation of definitive treatment. PET/MR imaging started with an average delay of 66±13 min after a body-weight adapted dosage (2 MBq/kg bodyweight) of 18F-FDG was injected intravenously. The MR-protocol comprised the following sequences: An axial diffusion-weighted EPI sequence and an axial T2w HASTE sequence. Furthermore, dedicated PET/MR imaging of the female pelvis comprised a sagittal and axial T2w TSE sequence and for dynamic imaging three repetitive scans of a T1w VIBE sequence after administration of i.v. contrast agent. Finally, a post-contrast fat-saturated T1w VIBE sequence for whole-body imaging was acquired (sequence parameters are given in figure 1). Image analysis of MRI and PET/MRI datasets was performed by a radiologist and a nuclear medicine physician, in consensus. The readers were instructed to determine the T-stage and to identify the manifestation of lymph node or distant metastases in each reading session. Sensitivity, specificity and diagnostic accuracy for each modality were calculated and a McNemar test was used to test for significant differences between the different ratings.
Results
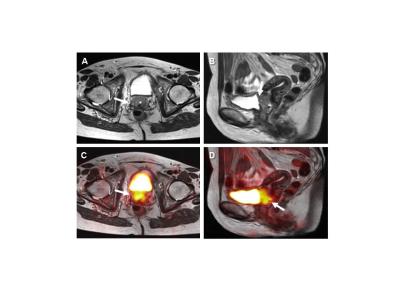
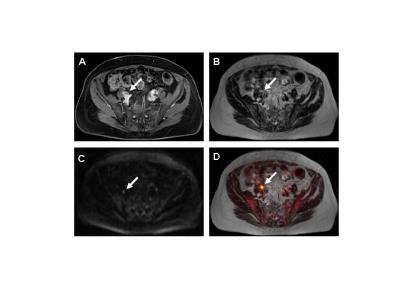
The histopathological types of the 47 primary cervical cancers were squamous cell carcinomas (n=37), Adenocarcinomas (n=9) and one Adenoid cystic carcinoma. The T-stage was determined for each patient and revealed one patient with stage IA, 21 patients with stage IB, 6 with stage IIA, 9 with stage IIB, one patient with stage IIIA and 5 patients with stage IIIB. Four additional patients were staged as IVA due to a histopathologically confirmed infiltration into the urinary bladder or rectum (figure 2). MRI enabled a correct identification of the T-stage in 41 (87%) out of the 47 patients. PET/MRI determined the correct T-stage in 40 (85%) cases. Furthermore, lymph node metastases were present in 22 (41%) out of 47 patients. For the identification of nodal positive patients PET/MRI showed higher values for sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy (86%, 92%, 91%, 89% and 89%) if compared to MRI alone (73%, 84%, 80%, 78% and 79%; figure 3). Finally, in 13 (28%) of the 47 patients distant metastases were present. Calculated sensitivity, specificity, PPV, NPV and diagnostic accuracy of PET/MRI (85%, 94%, 85%, 94% and 92%) showed higher values when compared to the results obtained with MRI alone (69%, 88%, 69%, 88% and 83%).Discussion
Our results demonstrate an equivalent diagnostic performance of PET/MRI and MRI alone for the determination of the T-stage of primary cancers of the uterine cervix. The utility of simultaneously acquired 18F-FDG PET data does not seem to provide useful additional information to MRI for the determination of the local extent of the primary tumors. Using PET/MRI, one additional patient with tumor stage IB was incorrectly classified as IIB, based on incorrect assumption of vaginal tumor invasion. Furthermore, the occurrence of lymph node or distant metastases at initial diagnosis has high impact on treatment planning and is considered an additional strong predictor for prognosis of cervical cancer patients. The present data show better results of simultaneously acquired 18F-FDG PET and MR data for the detection of nodal or distant metastases if compared to MRI alone. Accordingly, our results support the high diagnostic value of 18F-FDG PET data as part of hybrid imaging, thus offering a more accurate whole-body staging of cervical cancer patients.Conclusion
Integrated PET/MRI may serve as a valuable diagnostic modality for primary tumor staging of cervical cancer patients, providing useful information for therapy planning.Acknowledgements
No acknowledgement found.References
1. Bipat S, Glas AS, van der Velden J, Zwinderman AH, Bossuyt PM, Stoker J. Computed tomography and magnetic resonance imaging in staging of uterine cervical carcinoma: a systematic review. Gynecol Oncol. 2003;91(1):59-66.
2. Beckmann MW, Mallmann P, Uterus Commission of the Gynecological Oncology Working G. Interdisciplinary S2k guideline on the diagnosis and treatment of cervical carcinoma. J Cancer Res Clin Oncol. 2009;135(9):1197-206.
3. Kitajima K, Murakami K, Yamasaki E, Domeki Y, Kaji Y, Sugimura K. Performance of FDG-PET/CT for diagnosis of recurrent uterine cervical cancer. Eur Radiol. 2008;18(10):2040-7.
4. Antoch G, Saoudi N, Kuehl H, Dahmen G, Mueller SP, Beyer T, et al. Accuracy of whole-body dual-modality fluorine-18-2-fluoro-2-deoxy-D-glucose positron emission tomography and computed tomography (FDG-PET/CT) for tumor staging in solid tumors: comparison with CT and PET. J Clin Oncol. 2004;22(21):4357-68.
5. Grueneisen J, Schaarschmidt BM, Heubner M, Aktas B, Kinner S, Forsting M, et al. Integrated PET/MRI for whole-body staging of patients with primary cervical cancer: preliminary results. Eur J Nucl Med Mol Imaging. 2015;42(12):1814-24.
Figures