4803
Differentiating metastatic from nonmetastatic lymph nodes by using monoexponential, biexponential, and stretched exponential diffusion-weighted imaging in cervical cancer patients1Radiological Department, Henan Provincial People’s Hospital ( Zhengzhou University People’s Hospital ), Zhengzhou, People's Republic of China, 2MR Research China, GE Healthcare, Beijing, People's Republic of China, 3Pathological Department, Henan Provincial People’s Hospital ( Zhengzhou University People’s Hospital), Zhengzhou, People's Republic of China, 4Radiotherapeutical Department, Henan Provincial People’s Hospital ( Zhengzhou University People’s Hospital ), Zhengzhou, People's Republic of China
Synopsis
The aim of our study was to judge whether diffusion parameters derived from different models of multi-b value DWI could be used to discriminate metastatic from nonmetastatic pelvic lymph node (LN) status in patients with cervical cancer. A statistical significant difference in the mean D, f and α values between metastatic and nonmetastatic LNs, with metastatic LNs presenting with higher D values, lower f values and higher α values than nonmetastatic ones. This study revealed that metastatic LNs had their respective diffusion parameters compared with nonmetastatic LNs.
Purpose
Preoperative estimation of pelvic lymph node (LN) status is important to determine the treatment protocols in patients with cervical cancer. This study is to explore whether LN with high signal intensity on diffusion-weighted imaging (DWI) could be classified as metastatic or nonmetastatic, and to investigate the diagnostic value of diffusion parameters derived from monoexponential, biexponential, and stretched exponential models in cervical cancer.Method
A total of fifty female patients with cervical cancer were recruited including 39 early-stage and 11 advanced stage patients. All patients were scanned on a 3T MR750 scanner (GE Medical Systems, Milwaukee, Wis) using multi-b single shot SE-EPI pulse sequence with the following parameters: TR/TE=3200/110 ms, acceleration factor 2, slice thickness 3 mm with no gap and FOV 70×35, matrix size 96×64. Thirteen b-values set at 0, 50, 100, 150, 200, 300, 500, 800, 1000, 1300, 1500, 1700, 2000s/mm2 were acquired. Size parameters of LNs (Size-S, Size-L, S/L Ratio) and diffusion parameters (Dst, D, D*, f, DDC and α) calculated by fitting with monoexponential, biexponential and stretched exponential models respectively were compared between the metastatic and nonmetastatic LNs groups. All statistical analyses were performed with SPSS software. Receiver operating characteristic (ROC) curves were generated for each parameter to assess the area under the curve (AUC) and to determine which parameter was optimal for the differentiation of LNs. The sensitivity and specificity at the threshold values for each parameter were determined in the differentiation of LNs. Inter-observer agreement for the nodal parametric measurement was analyzed by calculating the intra-class correlation coefficient.Results
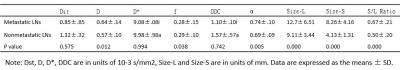
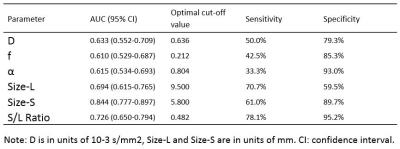
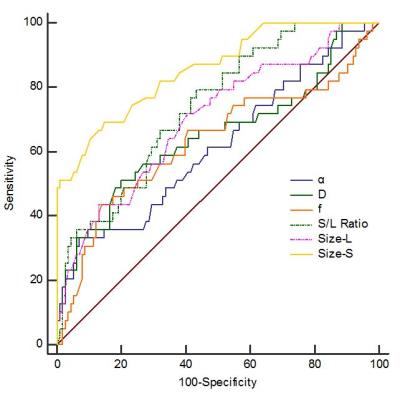
157 LNs with high signal intensity on multi-b value DWI was detected, and 41 of them were pathologically proved to be metastatic. Table 1 shows the quantitative comparison of the diffusion and size parameters between the nonmetastatic and metastatic LNs. The mean Size-L, Size-S and S/L Ratio of metastatic LNs were significantly higher than those of nonmetastatic LNs (P<0.05). The mean D and α value of metastatic LNs were significantly higher than those of nonmetastatic LNs. However, the mean f value of metastatic LNs was significantly lower than that of nonmetastatic LNs (P<0.05) (Figure 1). The ROC analysis indicated that size-s of LNs showed highest diagnostic value with AUC of 0.844, followed by S/L Ratio (0.726) and Size-L (0.694). Although the difference of D, f and α values existed between metastatic and nonmetastatic LNs, the diagnostic values of them were lower with AUC no more than 0.70 (Figure 2). Table 2 shows the sensitivity and specificity of the diffusion parameters at their optimal cut-off values for differentiating cervical cancer from normal cervix. The sensitivity for all parameters to detect metastatic LNs were no more than 80%. The value α showed the highest specificity of 93.0% in distinguishing LNs, but the sensitivity of it was extremely low.Discussion
The current results indicate that size parameters including the short and long diameter of LNs, S/L Ratio had significantly greater diagnostic properties than did diffusion parameters, including D, f, and α, in differentiating metastatic LNs from nonmetastatic LNs. In consistent with previous studies, the short diameter of LN still serves as the optimal parameter to characterize LNs in this study [1]. D values of metastatic LNs were significantly greater than those of nonmetastatic LNs, indicating increased water molecular diffusion within the metastatic LNs. This phenomena can be explained by the following reasons. First, tumor involvement changes the diffusion properties of malignant LNs. Secondly, necrosis is frequently seen in the LNs, especially in the larger ones, result in reduced cell density and large extracellular space, which facilitates the water movement. Thirdly, partial volume effect from adjacent nerve and vascular structure was unavoidable when we placed ROIs, especially for those smaller LNs. The f values of metastatic LNs were significantly lower than those of nonmetastatic LNs, indicating decreased micro-perfusion within the metastatic LNs, which is in consistency with one previous study in the evaluation of LNs in rectal cancer [2]. Previous studies reported that the D* values of metastatic LNs were statistically lower than that of nonmetastatic LNs, while this study did not find such difference [3, 4].Conclusion
In conclusion, this study revealed that metastatic LNs had their respective diffusion parameters compared with nonmetastatic LNs. D, f and α values showed statistical difference between metastatic and nonmetastatic LNs. The moderate AUC of D, f and α values indicated that they were less reliable to discriminate LNs compared with size parameters. Due to a limited sensitivity and specificity, diffusion parameters derived from multi-b value DWI are inferior to reliably discriminate metastatic from nonmetastatic LNs compared with size parameters in daily clinical routine.Acknowledgements
NoneReferences
[1] Liu Y, Liu H, Bai X, et al. Differentiation of metastatic from non-metastatic lymph nodes in patients with uterine cervical cancer using diffusion-weighted imaging. Gynecologic Oncology. 2011;122(1):19-24.
[2] Yu X-p, Wen L, Hou J, et al. Discrimination between Metastatic and Nonmetastatic Mesorectal Lymph Nodes in Rectal Cancer Using Intravoxel Incoherent Motion Diffusion-weighted Magnetic Resonance Imaging. Academic Radiology. 2016;23(4):479-85.
[3] Heijnen LA, Lambregts DM, Mondal D, et al. Diffusion-weighted MR imaging in primary rectal cancer staging demonstrates but does not characterise lymph nodes. Eur Radiol. 2013;23(12):3354-60.
[4] Liu C, Liang C, Liu Z, Zhang S, Huang B. Intravoxel incoherent motion (IVIM) in evaluation of breast lesions: comparison with conventional DWI. Eur J Radiol. 2013;82(12):e782-9.
Figures