4795
TRUS Biopsy Has a Lower Cancer Detection Rate in Large Prostate Volumes: Can In-Bore MRI-Guided Biopsy Do Better?1Radiology, Emory University-School of Medicine, Atlanta, GA, United States, 2Urology, Emory University-School of Medicine, GA, United States, 3Pathology, Emory University-School of Medicine, Atlanta, GA, United States
Synopsis
TRUS biopsy known to have low cancer detection rates in patients with large prostate volumes. With the proved advantages of MRI guided biopsy (MRGB), it may offer a better alternative to those patients. We compared between cancer detection rates of TRUS biopsy and MRGB in 49 patients as related to their prostate volumes. MRGB showed better detection of clinically significant cancers in prostate volumes between 30-59 mL . Adopting MRGB in patients with gland volumes ≥ 30 mL may save patients the need for repeated TRUS biopsies, provide better disease risk stratification, and reduce the healthcare costs associated with unnecessary biopsies.
Introduction and purpose:
Patients with large prostate volumes are frequently referred for transrectal ultrasound guided biopsy (TRUS-Bx) to investigate an elevated prostate specific antigen (PSA) level and/or an abnormal digital rectal exam (DRE). However, TRUS-Bx showed low cancer detection rates in this patient population, even when a larger number of biopsy cores is obtained 1-3. With the incremental shift of practice towards MRI targeted biopsy-owing to its better overall cancer detection rates and detection of clinically significant cancers with lower number of biopsy cores as compared to TRUS-Bx, 4-7 we hypothesize that MRGB may offer a better alternative for patients with large prostate volumes. The purpose of this study is to compare MRGB and TRUS-Bx in terms of overall cancer detection rates as well as clinically significant cancer (CSC) detection rates at various prostate volumes.Methods:
We retrospectively evaluated 64 consecutive prostate cancer patients who had both TRUS-Bx and MRGB and were diagnosed with prostate cancer by TRUS-Bx and/or MRGB. We excluded subjects who had negative biopsies after treatment and those with more than 24- month intervals between TRUS-Bx and MRGB. The final population included in this analysis was 49 patients. When TRUS-Bx and MRGB were concomitantly positive, the patient was assigned the result of the highest Gleason score (GS). For TRUS biopsy, at least 12 cores were obtained (range 12-16). All cases had mpMRI in a separate session prior to the targeted biopsy using 3T MRI scanner (Magnetom Trio, Siemens, Germany) with 32 channel surface phased array pelvic coil in supine position .High resolution axial, sagittal, and coronal Turbo spin echo (TSE) T2-WIs, Axial DWI (b-values=0, 1000, 1500 and 2000 s/mm2), DCE-MRI and pre- and delayed post-gadolinium VIBE scans. While the patient is prone, transrectal in bore MRI guided biopsy was performed on the same MRI scanner using the Dyna-TRIM/Dyna-CAD system (Invivo,Gainesville, FL) guidance . Targets were selected based on T2WI and DWI imaging appearance. We categorized prostate volumes as <30 cc, 30-59 cc, ≥60 cc. We compared these volume categories regarding overall and clinically significant cancer detection rates. For statistical analysis, we used McNemar’s test for paired nominal data and Fisher’s exact test other categorical data. Clinically significant cancers were defined as tumors having Gleason score ≥7.Results:
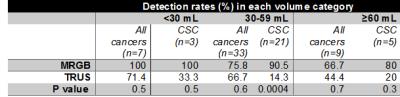
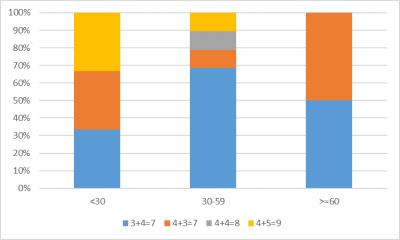
Most of the sampled prostate volumes were between 30-59 mL (33/49, 67.3%). Clinically significant cancers (≥3+4=7) were detected in 29/49 (59 %). Regarding all prostate cancers, there was no statistically significant difference in detection rates between MRGB and TRUS-Bx in all of the volume categories (i.e. <30, 30-59, and ≥60). Regarding clinically significant cancers (CSCs), MRGB showed a higher overall detection rate than TRUS-Bx (89.7 vs 17.2 % respectively) and a higher detection rate in prostate volumes ≥ 30 mL with detection rates of 88.5% vs 15.4 % respectively (McNemar test (Binomial distribution), p value = 0.0001). On further categorization, MRGB was also better than TRUS-Bx for detecting CSCs in prostate volumes between 30-59 mL (90.5 vs 14.3% respectively value = 0.0004). MRGB showed better detection of CSC than TRUS-Bx in prostate volumes ≥60 mL (80 vs 20 % respectively) but with no statistical significance , as illustrated in Table 1. TRUS-Bx missed 24/29 cases of CSC with the following grades: intermediate risk 3+4=7 (Grade group (GG) 2)- 66.7% (16/24), intermediate risk 4+3=7 (GG 3) -20.8% (5/24), high risk: 4+4=8 (GG 4) 4.2% (1/24) and 4+5=9 (GG 5) 8.3% (2/24). Most of patients with high risk disease were in the 30-59 mL volume group (figure 1). MRGB missed 3/29 cases of CSCs in the intermediate risk 3+4=7 (GG 2) 66.7% (2/3) and intermediate risk 4+3=7 (GG 3) 33.3% (1/3) grades.Conclusion:
In-Bore MRGB demonstrated a better detection rate for clinically significant cancers in patients with prostate volumes between 30-59 mL. Although it showed higher detection rate of CSCs in gland volumes ≥60 mL, it was statistically insignificant probably due to the small volume of that particular subset of the sample. Adopting MRGB in patients with elevated PSA levels and gland volumes ≥ 30 mL may save patients the need for repeated TRUS biopsies, provide better disease risk stratification, and reduce the healthcare costs associated with unnecessary biopsies.Acknowledgements
No acknowledgement found.References
1. Ung JO, San Francisco IF, Regan MM, DeWolf WC, Olumi AF. The relationship of prostate gland volume to extended needle biopsy on prostate cancer detection. J Urol. 2003;169(1):130-5.
2. Uzzo RG, Wei JT, Waldbaum RS, Perlmutter AP, Byrne JC, Vaughan ED, Jr. The influence of prostate size on cancer detection. Urology. 1995;46(6):831-6.
3. Karakiewicz PI, Bazinet M, Aprikian AG, Trudel C, Aronson S, Nachabe M, et al. Outcome of sextant biopsy according to gland volume. Urology. 1997;49(1):55-9.
4. Hambrock T, Somford DM, Hoeks C, Bouwense SA, Huisman H, Yakar D, et al. Magnetic resonance imaging guided prostate biopsy in men with repeat negative biopsies and increased prostate specific antigen. J Urol. 2010;183(2):520-7.
5. Felker ER, Lee-Felker SA, Feller J, Margolis DJ, Lu DS, Princenthal R, et al. In-bore magnetic resonance-guided transrectal biopsy for the detection of clinically significant prostate cancer. Abdom Radiol (NY). 2016;41(5):954-62.
6. Penzkofer T, Tuncali K, Fedorov A, Song SE, Tokuda J, Fennessy FM, et al. Transperineal in-bore 3-T MR imaging-guided prostate biopsy: a prospective clinical observational study. Radiology. 2015;274(1):170-80.
7. Geller RL, Nour SG, Osunkoya AO. Pathologic findings in patients with targeted magnetic resonance imaging-guided prostate needle core biopsies. Int J Clin Exp Pathol. 2015;8(9):9790-5.