4791
Ex vivo MRI evaluation of prostate cancer: localization and margin status prediction of prostate cancer in fresh radical prostatectomy specimens1Radiology and Nuclear Medicine, Radboud university medical center, Nijmegen, Netherlands, 2Pathology, Radboud university medical center, Nijmegen, Netherlands, 3Urology, Radboud university medical center, Nijmegen, Netherlands
Synopsis
This study investigated the ability of high field ex vivo MRI to localize prostate cancer (PCa) and to predict the margin status in fresh radical prostatectomy (RP) specimens using histology as gold standard. In twelve specimens, ex vivo MRI localized 17 (47%) of 36 PCa lesions confirmed by histological examination. Ex vivo MRI identified none of the 4 histological positive surgical margins (sensitivity 0%) and 9 of the 13 negative margins (specificity 69%). Our results indicate accurate localization of PCa in fresh RP specimens by ex vivo MRI, yet the technique did not perform well in predicting the margin status.
Introduction
Radical prostatectomy (RP) is the
recommended curative treatment in patients with low- and intermediate risk
localized prostate cancer (PCa) and a life expectancy of more than 10 years.1
At histological examination, tumor that extends to the inked surface of the
prostatectomy specimen is defined as a positive surgical margin (PSM) and is
considered an adverse patient outcome.2–4
Currently, indisputable and topical information on the margin status is
unavailable during or directly after surgery. Macroscopic evaluation by
palpation is unreliable and per-operative frozen section analysis (FSA) is
known to suffer from sample errors.5
Histological examination requires at least several days for a definitive
result. Until then, neither the surgeon nor the patient can be fully certain of
the treatment success. Acquiring ex vivo MR images of the RP specimen might be
a way to provide per-operative information on the margin status which could be
exploited to intraoperatively direct additional resection. This could
potentially decrease the number of PSM found at histological examination and
the subsequent need for radiotherapy or repeated surgery. In the present study,
the ability of high field ex vivo MRI to localize PCa and to predict the margin
status in fresh RP specimens is investigated.Methods
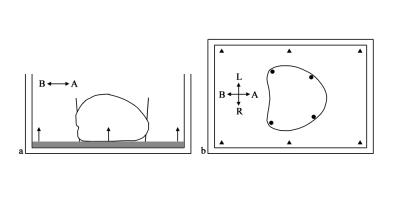
The
Institutional Review Board approved this study
and written informed consent was obtained. Patients with biopsy-proved PCa and
a multi-parametric MRI examination prior to undergoing RP were prospectively
included. Immediately after surgical resection, the entire intact prostate
specimen was positioned in a custom made container manufactured from MR compatible
acrylic glass that provided a reference between histological slicing and the ex
vivo MRI. The container with specimen was positioned in a 7 Tesla preclinical
MR scanner interfaced to a Siemens console. Turbo Spin Echo (TSE, TE/TR =
56/4,800, voxel size = 0.13x0.13x2 mm, matrix = 512x512) and half-Fourier
acquisition single shot turbo spin echo (HASTE, TE/TR = 44/2,000, voxel size =
0.51x0.51x2 mm, matrix = 128x96) with b-values of 0-100-500-1000-1200 s/mm2
sequences were applied to acquire T2 and diffusion weighted images
respectively. Furthermore, apparent diffusion coefficient (ADC) maps were
calculated. After the ex vivo MRI regular histological work-up followed. A
pathologist and a radiologist separately annotated areas of PCa and the
surgical margin status in the histology slides and ex vivo MRI respectively. Any
contact of a lesion visible on ex vivo MRI was defined as a PSM. The
radiologist determined the presence of PSM with a five-point Likert scale.Results
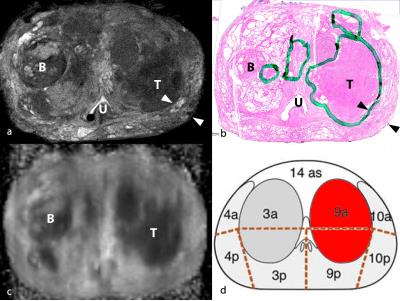
In
12 RP specimens, histopathology revealed 36 PCa lesions of which 17 (47%) were
correlated with a lesion annotated on the ex vivo MRI. The ex vivo MRI
localized 12 of 25 peripheral zone lesions (48%), 5 of 11 transition zone
lesions (45%), 10 of 24 Gleason score ≤ 6 lesions (42%), 7 of 12 Gleason score >
6 lesions (58%), 6 of 18 ≤ 0.5 cc lesions (58%), and 11 of 18 > 0.5 cc
lesions (61%). 7 of 11 (63%) Gleason score > 6 and > 0.5 cc lesion were
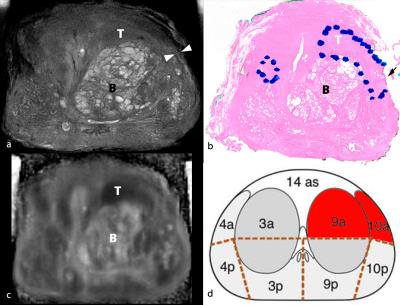
localized. The ex vivo MRI identified none of the 4 histological positive
surgical margins (sensitivity 0%) and 9 of the 13 negative margins (specificity
69%). The four false positive were assigned an average Likert score of 3.8 and
3.3, the four false negatives 2.0 and 1.8, and the true negatives 1.8 and 1.9 on
T2W and DW imaging respectively.
Discussion
To our knowledge, ex vivo MRI has never
been applied to localize PCa and predict margin status in fresh RP specimens.
This study demonstrated an overall localization rate for PCa of 47% which is
comparable with in vivo findings of Tan et al.6
The localization rate might improve with a more accurate correlation between
histology and ex vivo MRI. This could be achieved by improving the design of
the container limiting the variation of angulation of histological slicing. The
fact that a prostatectomy is sometimes performed maintaining a narrow margin (≈
1 mm) only might have resulted in the poor sensitivity of ex vivo MRI for PSM,
despite its high resolution (0.13x0.13x2 mm). The Likert scores for the false
positive surgical margin represent uncertainty of the reader.
Conclusion
Ex vivo MRI enabled accurate
localization of PCa in fresh RP specimens, yet the technique was unable to
provide indisputable information on the margin status. The ability of ex vivo MRI
to localize PCa might complement intraoperative frozen section analysis that
has a stronger performance to predict surgical margin statusAcknowledgements
Ex vivo MRI was performed using equipment of the Preclinical Imaging Centre (PRIME) within the Radboud university medical center, Nijmegen, the Netherlands.References
1. Heidenreich A, Bastian PJ, Bellmunt J, et al. EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent - Update 2013. Eur Urol. 2014;65(1):124–137.
2. Epstein JI, Amin M, Boccon-Gibod L, et al. Prognostic factors and reporting of prostate carcinoma in radical prostatectomy and pelvic lymphadenectomy specimens. Scand J Urol Nephrol Suppl. 2005;39(216):34–63.
3. Yossepowitch O, Bjartell A, Eastham J a., et al. Positive surgical margins in radical prostatectomy: outlining the problem and its long-term consequences. Eur Urol. 2009;55(1):87–99.
4. Yossepowitch O, Briganti A, Eastham J a., et al. Positive surgical margins after radical prostatectomy: a systematic review and contemporary update. Eur Urol. 2014;65(2):303–313.
5. Ramírez-Backhaus M, Rabenalt R, Jain S, et al. Value of frozen section biopsies during radical prostatectomy: significance of the histological results. World J Urol. 2009;27(2):227–234.
6. Tan N, Margolis DJ, Lu DY, et al. Characteristics of detected and missed prostate cancer foci on 3 T multiparametric MRI using an endorectal coil correlated with whole-mount thin-section histopathology. Am J Roentgenol. 2015;205(1):87–92.
Figures