4765
Non-iterative model for synthetic image-based registration of MOLLI cardiac T1 mapping images1Academic Radiology, University of Sheffield, Sheffield, United Kingdom, 2Pulmonary Vascular Disease Unit, Sheffield Teaching Hospitals NHS Trust, 3University of Cambridge
Synopsis
Cardiac T1 maps rely upon the acquisition of spatially aligned images. When patients fail to maintain breath hold, respiratory motion can cause T1 map inaccuracies due to poor image alignment. In the method demonstrated here, images are registered by co-registration to synthetic images, which are created via a non-iterative, automatic, model-based method. This method is compared to an iterative registration method using an energy minimisation process for quantitative registration accuracy and speed. Both methods were found to significantly improve image registration. The resultant registrations from both methods did not significantly differ, however the non-iterative model-based method reduced processing time by 1/5th.
Background
Cardiac T1 mapping is sensitive to changes in the myocardium due to disease. Accurate T1 mapping relies on spatially aligned images acquired during breath hold with cardiac gating. However, if a patient fails to maintain breath hold, respiratory motion can result in significant T1 map corruption. Various methods to compensate for motion during T1 mapping sequences have been employed, including co-registration of acquired images to synthetic images 1.Purpose
This work aims to evaluate a method of image registration that uses a non-iterative model-based approach to create synthetic images (method A) for the correction of cardiac motion in MOdified Look Locker Inversion (MOLLI) 2 imaging. Registration accuracy is compared to registration using synthetic images produced by an iterative combined approach to motion and T1 mapping using energy minimisation, based upon the work of Xue et al 1 (method B). Both methods were applied to MOLLI data from 19 cardiac patients and the results were compared in terms of quality of image co-registration and computational processing speed.Methods
19 patients were randomly selected from those who underwent a MOLLI T1 mapping sequence on a 1.5T GE HDx scanner as part of their clinical assessment at a pulmonary hypertension referral centre. Images were assessed visually for evidence of motion by an experienced cardio-thoracic radiologist. All images underwent both automated registration processes (A) and (B).
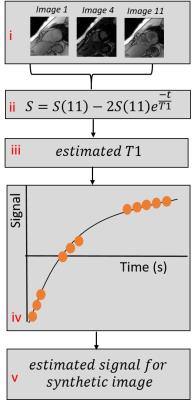
Method (A) was implemented in Matlab, and uses a simplified inversion recovery model to create spatially-aligned synthetic images, to which the acquired images are co-registered, after which T1 maps are produced separately, see Figure 1. Method (B) was implemented in Matlab based on the work of Xue et al., 2014 1, and employs an iterative energy minimisation process to collectively reduce motion in the acquired images and calculate T1 maps.
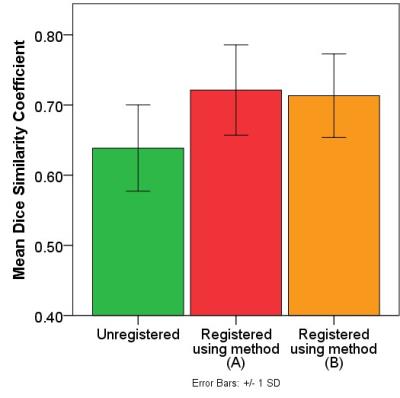
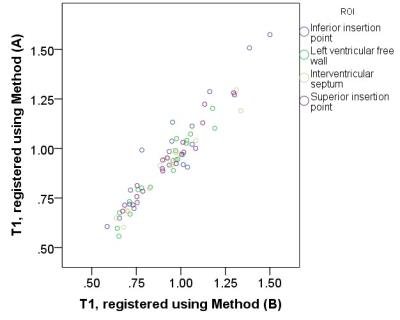
Image co-registration quality was quantitatively assessed using the Dice similarity coefficient (DSC) 3. DSC values were calculated using the segmented left ventricle of the first 9 MOLLI image acquisitions (images 10 and 11 did not have sufficient blood-myocardium contrast for segmentation). Conservative, central regions of interest were drawn onto post-registration T1 maps to establish whether both methods produced consistent T1 values. Resultant T1s were compared for consistency using a correlation coefficient for absolute agreement and Bland-Altman analysis.
Results
17/19 patients were found to have some myocardial motion present in their acquired MOLLI images. In 5/19 patients, motion was considered to be moderate to severe.
Registration methods (A) and (B) both resulted in significantly improved registration of the images in the whole cohort, as quantified by a significantly higher DSC value post-registration (paired t-test A: P<0.001; B: P<0.001), see Figure 2.
The mean T1 of myocardial regions in the post-registration T1 maps was not significantly different between the two registration methods, see Figure 3.
The iterative nature of the energy minimisation in method (B) resulted in longer processing times; the average time for post-registration analysis using method (A) was 1/5th of that required for (B) (226±4 minutes compared to 1136±19 minutes).
Conclusion
Both methods (A) and (B) significantly improved the spatial registration of MOLLI images in this cohort. There was no significant difference in registration success between the two methods, however method (A) required less processing time.
Although the processing times of method (B) were longer than those presented by Xue et al., 2014 1, both method (A) and (B) were implemented in Matlab with identical code for common processes. Due to the non-iterative nature of method (A), it is expected that this method would maintain reduced speed in more computationally efficient implementations of both of these methods.
Acknowledgements
No acknowledgement found.References
1. Xue, H., et al., Motion correction for myocardial T1 mapping using image registration with synthetic image estimation. Magn Reson Med, 2012. 67(6): p. 1644-55.
2. Messroghli, D.R., et al. Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med, 2004 . p141-6.
3. Zou, K.H., et al., Statistical validation of image segmentation quality based on a spatial overlap index. Academic radiology, 2004. 11(2): p. 178-89.
Figures