4722
Triple Magnetic Resonance Angiography (triple-MRA) for planning of Gamma Knife Radiosurgery of brain arteriovenous malformations1The Gamma Knife Centre at Queen Square, National Hospital for Neurology and Neurosurgery, London, United Kingdom, 2Department of Neurosurgery, National Hospital for Neurology and Neurosurgery, London, United Kingdom, 3Medical Physics and Biomedical Engineering, University College London, London, United Kingdom, 4Academic Neuroradiological Unit, Department of Brain Repair and Rehabilitation, Institute of Neurology, University College London, London, United Kingdom, 5The Lysholm Department of Neuroradiology, National Hospital for Neurology and Neurosurgery, London, United Kingdom, 6C. J. Gorter Center for High Field MRI, Department of Radiology, Leiden University Medical Center, Leiden, Netherlands, 7Centre for Medical Imaging, University College London, London, United Kingdom
Synopsis
This study investigates whether a combination of three MRA techniques, referred to as triple-MRA, could be used as an alternative to DSA for visualisation and delineation of brain AVMs for GKR targeting. The AVMs of 13 patients undergoing GKR were delineated using triple-MRA and the resultant target volumes were compared to the radiosurgical targets generated by the neurosurgical team using DSA and volumetric contrast T1/T2 imaging. Target volumes obtained using triple-MRA are comparable to target volumes obtained with DSA and used for delivery of GKR. In conclusion, triple-MRA is a robust method for non-invasive identification and delineation of brain AVMs.
Objective
Gamma Knife Radiosurgery (GKR) is a well-established minimally invasive treatment for selected cases of brain ArterioVenous Malformations (AVMs).1 The state-of-the-art planning strategy for GKR of brain AVMs involves an intra-arterial Digital Subtraction Angiography (DSA) on the day of treatment for delineation of the radio-surgical target, as well as standard volumetric MRI scans.2 However, DSA is invasive. It carries a potential risk of peri-procedural complications and exposes both patients and staff to ionizing radiation.3
This study aims to evaluate whether a combination of three Magnetic Resonance
Angiography (MRA) techniques, referred to as triple-MRA, could be used as an
alternative to DSA for visualisation and delineation of brain AVMs for GKR
targeting.
Methods
Thirteen patients undergoing DSA for targeting of GKR for brain AVMs also underwent triple-MRA including: 4D Arterial Spin Labelling based angiography (4D-ASL-MRA), High Definition Time-Of-Flight angiography (HD-TOF) and Contrast-Enhanced Time-Resolved MRA (CE-TR-MRA).
Nine patients presented
with intracranial bleeds and two with seizures. The AVM was incidentally found
in two subjects. Three of the patients had undergone partial glue embolization
before GKR. The AVMs were well distributed across the head anatomy (parieto-occipital:5,
temporal/basal ganglia:4, frontal:3, cerebellar:1). The mean AVM target volume, as drawn by the
neurosurgical team for delivery of GKR using 2D projections of DSA into volumetric
contrast T1 and T2 imaging (DSA volume), was 3.4 ml (0.1-8.3).
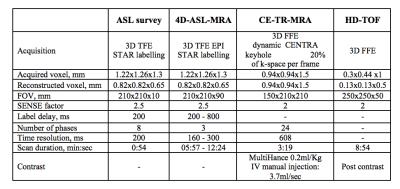
Triple-MRA was performed using a 3.0T MRI system (Philips Healthcare Systems, The Netherlands) and the parameters in table 1. An ASL-MRA based vascular survey with 200 ms temporal resolution was used to characterise the filling velocity of the AVM in each individual case. This survey was used to identify the three time points that best depicted the arterial and nidus phases of the AVM and to tailor the timing of 4D-ASL-MRA. For this reason, triple-MRA scanning time varied among patients between 19.04 and 25.31 minutes.
Triple-MRA datasets, along with volumetric post-contrast T1 and T2 MRI scans used for GKR planning, were transferred to the Brainlab Elements platform (Brainlab AG, Feldkirchen, Germany) for post-processing. This involved image co-registration, automatic blood vessel segmentation on HD-TOF, generation of Maximum Intensity Projections and delineation of the AVMs using the semi-automatic drawing tool AngioBrush. The arterial phase of the AVM nidus excluding draining veins was then delineated (ARV) using triple-MRA and volumetric post-contrast T1 and T2 MRI. This was achieved by including in the triple-MRA volume the areas shown to be part of the AVM nidus in all three MRA techniques as well as standard volumetric MR imaging. Target volumes generated using triple-MRA can be exported into the GKR planning system in DICOM RT structure format for treatment delivery. The degree of overlap between DSA and triple-MRA was calculated using HorosTM (LGPL 3.0).
Results
The AVM nidus was clearly identified on all three MRA techniques in eleven cases. In one case the lesion was depicted on CE-TR-MRA and HD-TOF but not on 4D-ASL-MRA most likely due to the posterior and superficial location of the lesion (occipital lobe) with the ASL labelled blood losing its labelling before filling the AVM. In another case, the acquisition did not include the arrival of the gadolinium bolus and therefore it was not possible to visualize the AVM on CE-TR-MRA; it was, however, clearly depicted on HD-TOF and 4D-ASL-MRA.
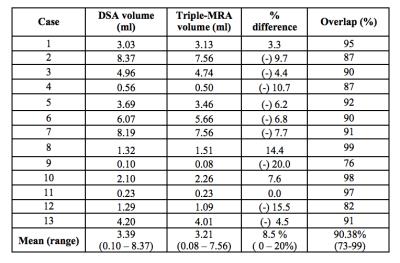
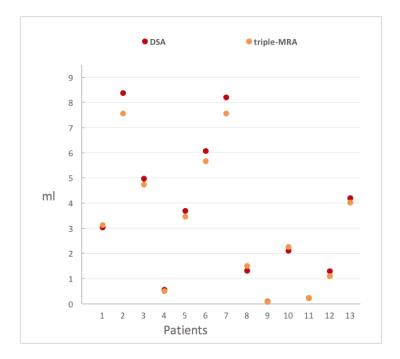
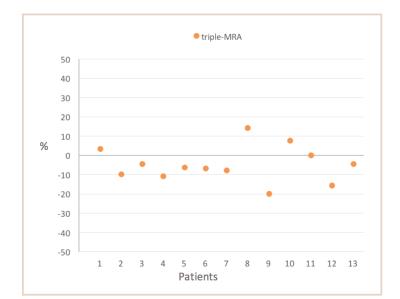
Figure 1 shows the DSA and triple-MRA target volumes for each patient. The mean percentage difference between DSA and triple-MRA target volumes was 8.5%; range: 0-20% (table 2). The percentage difference between DSA and triple-MRA volumes was below 15% in all cases but one (case 9) in which a small variation in volumes represented a high percentage difference due to the very small size of the target (0.1 ml), figure 2.
The overlap between DSA and triple-MRA volumes, defined as the percentage of the DSA volume included in triple-MRA volume, was 90.38% on average (table 2). It was above 80% in all subjects except for case 9, for the same reason stated above. Triple-MRA volumes were smaller than DSA volumes in 70% of the cases.
Discussion
The combination of three MRA techniques is a robust method for non-invasive identification and delineation of brain AVMs. When used in combination, HD-TOF, 4D-ASL-MRA and CE-TR-MRA can provide target volumes which are comparable (or 8.5% smaller on average) to target volumes obtained with DSA and used for delivery of GKR.Conclusions
Triple-MRA provides AVM volumes that are comparable to radiosurgical target volumes drawn using DSA and it is a reliable, non-invasive alternative for visualisation and delineation of brain AVMs for GKR targeting.Acknowledgements
This project was funded by The National Brain Appeal and the EPSRC (First grant EP/K027476/1 awarded to Karin Shmueli). The Brainlab AG provided the Elements software free of charge for triple-MRA post-processing.References
1. Pollock BE, Link MJ, Stafford SL, Garces YI, Foote RL. Stereotactic Radiosurgery for Arteriovenous Malformations: The Effect of Treatment Period on Patient Outcomes. Neurosurgery. 2016;78(4):499-509.
2. Seymour ZA, Sneed PK, Gupta N, Lawton MT, Molinaro AM, Young W, et al. Volume-staged radiosurgery for large arteriovenous malformations: an evolving paradigm. J Neurosurg. 2016;124(1):163-74.
3. Kaufmann TJ, Huston J, 3rd, Mandrekar JN, Schleck CD, Thielen KR, Kallmes DF. Complications of diagnostic cerebral angiography: evaluation of 19,826 consecutive patients. Radiology. 2007;243(3):812-9
Figures