4692
MRI to monitor the impact of positional changes in the airway of sleep apnea patients – A Phase I methodology demonstration at 3T1Wright Center of Innovation in Biomedical Imaging, Department of Radiology, The Ohio State University, Columbus, OH, United States, 2Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine, The Ohio State University, Columbus, OH, United States, 3Hill-Rom
Synopsis
We aimed to develop a non-invasive quantitative MRI methodology to assess positional and rotational impact on the airway opening in subjects with history of sleep apnea for a proposed clinical trial. An equipment and software analysis approach was implemented to perform a feasibility demonstration using 9 volunteers. All data analysis was performed on IntelliSpace Portal (ISP) (Philips Healthcare) to validate the angles and perform the assessment of the airway opening in the RP and RG regions. We have established a prototype table setup that enables us to image 7 positions of various head and chest support angles to investigate the best positional changes to improve the airway opening of sleep apnea subjects. The results showed that the actual angles were within 0.10-0.30 from the targeted angles. In conclusion, the developed 3T MRI methodology appears robust to assess the impact of head and chest positional changes on the airway in sleep apnea patients.
Purpose
While the impact of position in sleep is well recognized, MRI was seldom used to objectively assess how positional changes impact the airways. We embarked to develop a non-invasive, quantitative MRI methodology to assess positional and rotational impact on the airway opening in subjects with history of sleep apnea for a proposed clinical trial.Methods
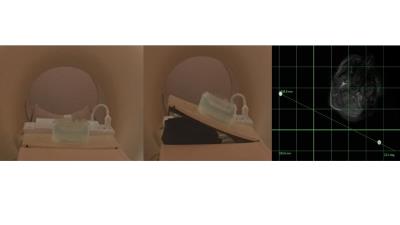
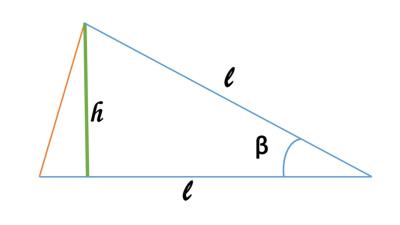
After a multi-disciplinary project design development, we implemented an equipment and software analysis approach and performed a feasibility demonstration using 9 volunteers. Subjects were positioned in the supine position on the MRI table. In order to facilitate the independent rotational changes of the patient’s head and chest, two separate plates were hinged on the left side of the MRI table top. Under each plate we placed a special balloon (called a bladder) that could be inflated or deflated by an airpump system from outside the magnet room to rotate the plates in the z-direction (along B0 field) (Figure 1). To track the angles of rotation, a set of 2 vial tubes filled with contrast agent solution were placed on each plate and below the cushion pad (Figure 1). To tilt a plate at a targeted angle, the plate was raised at the associated height (Figure 2).
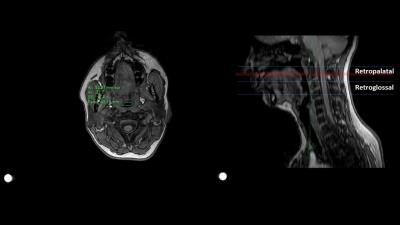
Phantom and volunteer scans have been utilized to optimize the MRI protocol. All MRI scans were performed on a 3T system (Ingenia CX, Philips). To determine and confirm the angle at which the two plates were tilted, a fast 2-D T1-weighted FFE sequence (TR/TE (ms), 3.1/1.5; in-plane FOV (mm), 530x530; number of stacks, 2; stack FH (mm), 172; voxel size (mm), 1.0/1.0/40.0; flip angle, 100; scan time (s), 30) that covered the lower part of the head and upper part of the chest was performed (Figure 1) in the transverse direction using the body coil. Subsequently, a high resolution 3-D T1W FFE sequence (TR/TE (ms), 3.2/1.7; in-plane FOV (mm), 400x400; FH (mm), 230; voxel size (mm), 1.0/1.0/2.0; flip angle, 100; scan time (s), 150; slice orientation was matched with the angle of the plate) was performed in the transverse orientation to image the regions of interest (ROIs) which are retropalatal (RP) and retroglossal (RG) sections of the airway (Figure 3) with the anterior 16-channel cardiac coil placed on the head plate, thus rotated with the plate (Figure 1).
All data analysis was performed on IntelliSpace Portal (ISP) (Philips Healthcare) to validate the angles of the plates and perform the assessment of the airway opening. The cross-sectional area, lateral distance, and anterior-posterior distance of the airway on each slice in the RP and RG regions were chosen as desired assessment parameter.
Results
A prototype table setup has been developed that enables to change the rotational position of subjects inside an MRI room. Using the ISP software, the measurement of tilted angles of head and chest rotations showed that the actual angles were within 0.10-0.30 from the targeted angles. For each set of 2 angles (one for the head and one for the chest), the set-up time could be done within 4 minutes and the scan time was within 4 minutes, allowing the total time of less than 10 minutes. Therefore, the protocol was built to image 7 positions of various head and chest support angles to investigate the best positional changes to improve the airway opening of sleep apnea subjects.
The 3T MRI protocol gave an excellent visualization of the airway, which enables automatic ROI placement (auto contour) to provide the most objective measurement of cross-sectional area, lateral distance, and anterior-posterior distance of the airway (Figure 3). There was a sharp contrast of the airway with the surrounding tissues including soft palate and epiglottis.