4666
Positional variation of parotid glands in the treatment position of head and neck radiotherapy with immobilization: a pilot study on healthy volunteers using high spatial resolution 3D MRI at 1.5T1Medical physics and research department, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong, 2Department of Radiotherapy, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
Synopsis
Investigation of positional and geometric variations of organ-at-risk (OAR) in head-and-neck (HN) radiotherapy (RT) is greatly limited by the poor soft tissue contrast of X-ray-based imaging. We investigated the positional variation of parotid glands (PG) in the immobilized HN-RT treatment position on healthy volunteers using high-spatial-resolution 3D-MRI at 1.5T. The results showed that PGs generally had sub-millimeter and sub-degree group mean error, systematic error and random error under immobilization. Although PGs generally showed insignificant positional variations from global HN, individual left and right PG might move independently and resulted in insignificant positional correlations with each other and global HN.
PURPOSE
Patient setup protocol currently used in radiotherapy (RT) practice is based on the assumption of rigid body motion and bones on X-ray based imaging are used as surrogate of target and organ-at-risks (OAR) for patient setup correction. Head-and-neck (HN) is a complex site for radiotherapy with high geometrical uncertainties even after tight immobilization, treatment margin setting and setup error correction (1). Investigation of positional and geometric variations of target and OARs in HN-RT is greatly limited by the poor soft tissue contrast of X-ray based imaging. MRI has potentials on geometric uncertainty reduction for HN-RT by taking the advantages of superior soft tissue contrast. This pilot study aimed to investigate the positional variation of parotid glands, an important OAR with high probability of complication after HN-RT (2), in the immobilized HN-RT treatment position on a cohort of healthy volunteers using high spatial resolution 3D MRI.METHODS
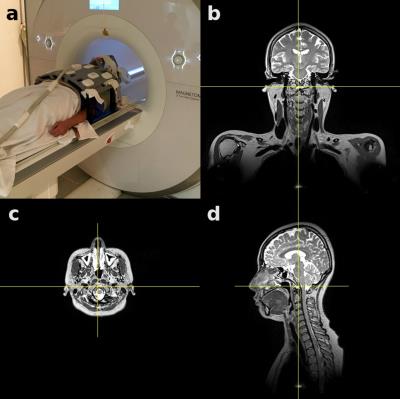
12 healthy volunteers were recruited and each received four MRI scans on a 1.5T MRI simulator (MR-sim) with a flat couch top. Subjects were each time repositioned, immobilized with 5-point thermoplastic mask (with reference lines for alignment) routinely used in HN-RT, and aligned with a 3D external laser to minimize positional variability between scans. Two 6-channel flexible coils, an 18-channel body coil and spine coil were used for reception without touching subjects (Fig. 1). A 3D T1w SPACE sequence enabling 3D geometric distortion correction (TE/TR=7.2/420ms, turbo factor=40, isotropic voxel size=1.05mm, GRAPPA factor=3, bandwidth=657Hz/pixel, acquisition time=5min) was used for acquisition. Acquired images were processed using 3D slicer. Four anatomies of left PG only (PGl), right PG only (PGr), both parotid glands (PGs) and global head and neck caudal to thoracic spine T3 (HN) were outlined and their positional variations were assessed. Transformation matrics were calculated through rigidly registering the images of each anatomy to the reference images obtained in the first scan, and then used to derive translations and rotations. Group mean error (M), systematic error (Σ) and random error (σ) of each anatomy were quantified (3). Positional variation differences between anatomies were compared using paired t-test and positional variation correlations between anatomies were assessed using Pearson correlation coefficient r.RESULTS
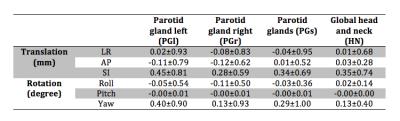
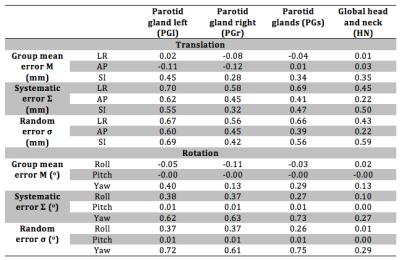
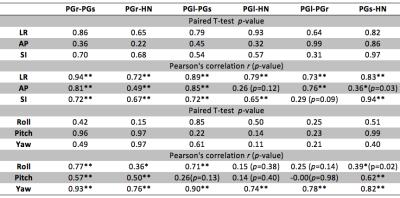
Positional variations of four anatomies were summarized (Table 1). Systematic error and random error of all anatomies were smaller than 1mm and 1o, of which PGl had the largest Σ and σ in three translational directions (Table. 2). Paired t-test (Table.3) showed that translations and rotations between any two anatomies were not significantly different. All four anatomies mostly exhibited significantly high correlations on positional variations (Table. 3), but insignificant positional correlations were also found. For instance, insignificant translation correlation was found in AP between PGl and HN (r=0.26, p=0.12) and in SI between PGl and PGr (r=0.29, p=0.09), and insignificant rotation correlation in roll (r=0.15, p=0.38) and pitch (r=0.14, p=0.40) between PGl and HN.DISCUSSION
By taking the advantage of superior soft tissue contrast and isotropic small voxel size, positional variations of PGs was accurately assessed without bias in different dimensions. Results showed sub-millimeter translation and sub-degree rotation in PG and global HN could be achieved under immobilization on a MR-sim. Although insignificant positional variation differences and highly correlated positional variations were exhibited in general, our results did show the different positional variability between PGl and PGr, indicating the independent motion of individual parotid gland. Due to motion flexibility and deformability of soft tissues, global HN used as positional surrogate might not accurately represent positional variability of individual soft tissues like parotid glands, resulting in potential residual positional errors. In this aspect, MRI has potentials to provide a tissue-specific positional verification and correction method to guide HN-RT in the future. This study has limitations. Besides small sample size, positional variability might be underestimated on healthy volunteer data in the absence of patient weight loss, tumor shrink, parotid gland shrink and/or deformations during treatment. Rigid image registration could not accurately assess the possible PG deformations, which was assumed to be negligible in normal PGs but yet to be validated. This study did not study the relationship of positional variations between PG and hard tissues that are routinely used for positional verifications in HN-RT. Residual geometric distortion of MR images was not considered.CONCLUSION
Parotid glands generally had sub-millimeter and sub-degree positional variations in the immobilized treatment position of HN-RT as revealed by high resolution T1w 3D MRI, showing no significant difference from global HN positional variations. Individual left and right PG could have insignificant positional correlations with each other and global HN.Acknowledgements
No acknowledgement found.References
1. van Kranen, Simon, et al. "Setup uncertainties of anatomical sub-regions in head-and-neck cancer patients after offline CBCT guidance." International Journal of Radiation Oncology* Biology* Physics 73.5 (2009): 1566-1573.
2. Kam, Michael KM, et al. "Prospective randomized study of intensity-modulated radiotherapy on salivary gland function in early-stage nasopharyngeal carcinoma patients." Journal of Clinical Oncology 25.31 (2007): 4873-4879.
3. Van Herk, Marcel. "Errors and margins in radiotherapy." Seminars in radiation oncology. 14.1 (2004):52-64.
Figures