4661
B0 and B1 Field Inhomogeneity Consideration in Pseudo-continuous ASL Due to the Presence of Carotid Artery Stenting1GE Healthcare, Taipei, Taiwan, 2GE Healthcare MR Research China, Beijing, People's Republic of China, 3Department of Radiology, Taipei Medical University - Shuang Ho Hospital, New Taipei City, Taiwan
Synopsis
Pseudo-continuous arterial spin labeling (pCASL) has been recently used for investigating cerebral hemodynamic change on the patient receiving carotid artery stenting (CAS) because it permits repeated measurement of absolute cerebral blood flow in a short interval without MR contrast agent or radioactive material. However, labeling efficiency of pCASL has been proved to be dependent on B0 and B1 inhomogeneity. The aim of this study was to understand how inhomogeneous of the B0 and B1 at labeling position of pCASL and find the remedies of the pCASL measurement for the CAS patient.
Purpose
Carotid artery stenting (CAS) is being increasingly used as an alternative treatment to carotid endarterectomy for carotid artery stenosis1. Variable imaging modalities have been applied to investigate cerebral hemodynamic change after CAS2. However, it remains unclear which hemodynamic changes occur in certain areas of the brain following CAS. Pseudo-continuous arterial spin labelling (pCASL) is an emerging MRI method for studying cerebral perfusion using radiofrequency (RF) pulses for the noninvasive labeling of endogenous water protons in the blood3 instead of injecting exogenous contrast agent or radioactive material. This technique is capable of detecting absolute cerebral blood flow (CBF) at the brain tissue level (ml/100g per minute) permits repeated measurement of CBF in a short interval, which is useful in patients receiving CAS4. However, the labeling process of pCASL is not strictly an adiabatic inversion and the labeling efficiency may be dependent on B0 and B1 inhomogeneity or other factors5, which are especially concerns for CAS patient. The aim of this study was to understand how heterogeneous of B0 and B1 field caused by stent at labeling region of pCASL and find the solution without compromising the pCASL measurement in the CAS patients.Methods
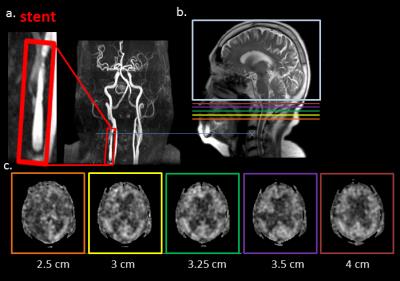
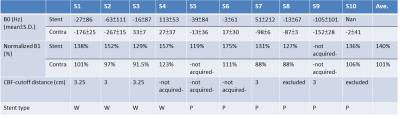
Ten patients with symptomatic internal carotid artery stenosis receiving CAS were included in the study. Two stent types (Boston Wallstent® and Cordis Precise®) were used in these CAS treatment patients. All MRI acquisitions were performed on a 3T clinical scanner (Discovery MR750, GE Healthcare) using an 8-channel brain coil as signal detection and whole body coil for RF excitation. Perfusion study was conducted using a pCASL with a TR=5327 ms, an TE=10.5 ms, FOV=24×24 cm, labeling duration=1.5 s, post labelling delay=2525 ms, matrix=128×128, NEX=2, slice thickness =4 mm. In addition, labelling plane was 3.35-mm thick and placed at 2.18 cm inferior to the lower edge of the scanning coverage. The CBF maps were generated on an Advantage Windows workstation (version 9.4, GE Healthcare). For identifying stent position, time-of-flight magnetic resonance angiography (TOF-MRA) was acquired. Coronal B0 map of the tagging region was acquired by two gradient echo images with a TE difference of 1.5 ms, while B1 map was acquired by gradient echo Bloch-Siegert sequence with a TR of 19 ms, an TE of 12.8 ms, a matrix of 128×128, and a pair of Fermi pulses (8 ms duration) having off-resonace +/-4 kHz6. To determine the optimal labeling position, the distance between stent and labeling plane was varied to be 2.5, 3, 3.25, 3.5, 4 cm.Results
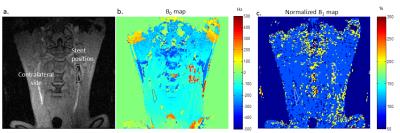
Stent position can be identified by coronal gradient-echo images with hypointensity (Fig. 1a). B0 and normalized B1 maps were shown in Fig. 1b and Fig. 1c, respectively. Quantitative measurement of B0 and B1 value at each patient was summarized at Tab. 1. Part of data was excluded due to the bad quality from motion or other reason. B0 field at stent region appeared rather inhomogeneous according to the B0 map and its quantitative data with high standard deviation, ranging from ±53 to ±212 Hz. B1 measurement by acquiring the Block-Siegert phase shift between two scans is independent of B0. Normalized B1 was calculated by a ratio of actual nominal flip angle (Fig. 1c and Tab. 1) and it is found to be higher than desired (140%) on stenting side and close to actual flip angle (101%) on contralateral side. The estimated CBF map (Fig. 2) showed the lower CBF at ipsilateral hemisphere and back to normal compared to contralateral side as the labeling position of pCASL away from stent. CBF-cut-off distance (Tab.1) suggested that the CBF recovered to normal level at 3.25 cm of the distance between stent and labeling position.Discussion and Conclusion
Noncontrast pCASL method is very useful for evaluating cerebral hemodynamic change on the patient after CAS. However, prominent frequency incoherence and B1 inhomogeneity due to the presence of stent (Fig. 1 and Tab. 1) would substantial reduce the labeling efficiency and thus cause quantification error for pCASL if the labeling plane at or close to the stent position. The quantification error caused by the combination of B0 and B1 inhomogeneity could not be easily compensated. Alternatively, we demonstrated that perfusion signal would not be compromised when labeling position is 3.25 cm away from stent position (Tab. 1 and Fig. 2). It is advised that the distance may vary with different type of stent materials7. Nonetheless, once the optimal labeling distance has been determined in the first time of pCASL experiment for the material, the same acquisition condition can be applied to CAS patient with the same stent.Acknowledgements
No acknowledgement found.References
1. Brott TG, Hobson 2nd RW, Howard G, et al., “Stenting versus endarterectomy for treatment of carotid-artery stenosis,” N Engl J Med, 363(1):11-23, 2010
2. Chang TY, Liu HL, Lee TH, et al., “Change in cerebral perfusion after carotid angioplasty with stenting is related to cerebral vasoreactivity: a study using dynamic susceptibility-weighted contrast-enhanced MR imaging and functional MR imaging with a breath-holding paradigm,” AJNR Am J Neuroradiol, 30:1330–1336, 2009.
3. Wang JJ, Alsop DC, Li L, et al., “Comparison of quantitative perfusion imaging using arterial spin labelling at 1.5 and 4.0 tesla,” Magn Reson Med, 48(2):242-54, 2002
4. Chen YT, et al., “Loss of labelling efficiency caused by carotid stent in pseudocontinuous arterial spin labelling perfusion study,” Clinical Radiology, 71:e21-e27, 2016.
5. Jahanian H, et al., “B0 field inhomogeneity considerations in pseudo-continuous arterial spin labeling (pCASL): effects on tagging efficiency and correction strategy,” NMR in Biomed, 24: 1202–1209, 2011
6. Sacolick L, et al., “ B1 Mapping by Bloch-Siegert Shift,” Magn Reson Med, 63(5):1315-22, 2010.
7. Lin CY, et al., “Experimentally optimizing labeling position in pseudo-continuous ASL in the presence of carotid artery stenting,” The proceeding of ISMRM, p4111, 2016
Figures