4621
Voxel-based Lesion Mapping of Cardiogenic Cerebral Embolism1Neurosurgery, Kawachi general hospital, Higashi Osaka, Japan, 2Neurosurgery, Osaka Medical Center for Cancer and Cardiovascular Diseases, Osaka, Japan
Synopsis
Although outcome of acute cardiogenic cerebral embolism patients improved dramatically due to development of interventional devices, sub-acute cases over the golden period still follow miserable clinical courses requiring to elucidate the pathology of cerebral ischemia. The authors attempted to unveil the correlation of clinical features following cardiogenic cerebral embolism and the locations or sizes of the infarction using voxel-based lesion mapping (VBLM). Our result revealed a correlation between spatial characteristics of infarction and clinical features. Larger ischemic volume at the left hemisphere is correlated with patient’s outcome and cerebral herniation was strongly influenced by ischemic volume after standardization.
Introduction
Recently, outcome of acute cardiogenic cerebral embolism patients improved dramatically due to development of interventional devices1. However, sub-acute cases over the golden period still follow miserable clinical courses, which raises the importance to elucidate the pathology of cerebral ischemia. In this report, the authors attempted to unveil the correlation of cerebral herniation following cardiogenic cerebral embolism and the locations or sizes of the infarction using voxel-based lesion mapping technique (VBLM), similar to the methods that the authors have reported on brain tumors2.Materials and Methods
Patient selection This study was a retrospective data analysis of patients who were treated as a cardiogenic cerebral embolism from January 2011 to December 2014. ASCO grading was used to diagnose cardiogenic cerebral embolism3. The inclusion criteria were patients who had grade 1 evidence of only C (cardiac diseases) phenotype, and underwent MRI within a few days after onset of stroke. Voxel-based lesion mapping Diffusion weighted image (DWI) hyper-intense lesions in each case was segmented in 3D as voxels-of-interest (VOI). Alongside to this process, DWIs were standardized to the human brain MRI atlas provided by the Montreal Neurological Institute (MNI 152) providing the transformation matrixes. VOIs were then subsequently transformed to MNI152 space using the transformation matrixes. A lesion map was created by accumulating the VOIs on MNI152. The patient cohort was divided into subgroups according to the outcome (mRS 0-2 or 3-6) or presence of midline shift indicative of cerebral herniation (>10mm). The lesion maps were visually and statistically compared between each subgroup.Results
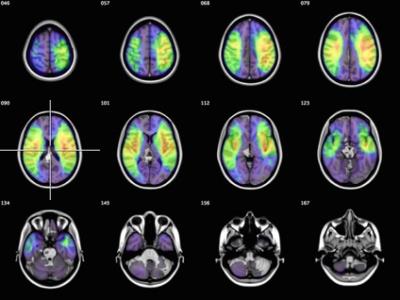
Ninety patients were included in our analysis. The mean age
of patients was 75.9 years. The lesion map of all cases revealed ischemic
lesions accumulating at bilateral middle cerebral artery territories,
especially involving the primary motor cortex (Fig.1). Ischemic volumes at each
hemisphere after standardization were 103.9ml (n=63) at the right side and
131.9ml (n=61) at the left side (p>0.05). The lesion map for favorable clinical
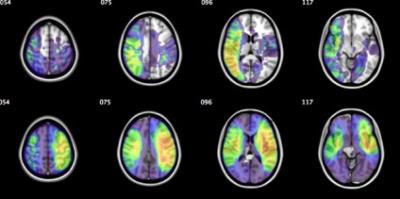
outcome subgroup showed that the lesions accumulated at the right parietal
lobe, whereas the left parietal lobe was correlated with poor clinical outcome (Fig.2).
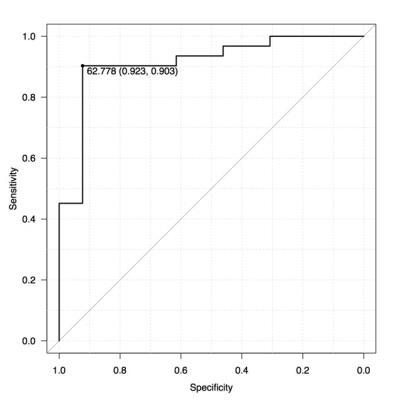
On left hemisphere, ischemic volume after standardization was positively
correlated with mRS, and ROC analysis revealed poor outcome over 62.8ml
(AUC=0.91, sensitivity=0.923, specificity=0.903) (Fig.3). The ischemic lesions
for the subgroup that experienced midline shift group showed left-sided, wide
spread lesions and ischemic volume after standardization of midline shift subgroup
was significantly larger than those with no midline shift (p<0.05).Discussion
Previous studies reported right hemisphere propensity for cardiogenic embolism4,5. The present data, however, did not show obvious laterality between ischemic volumes at the left and right side. The lesion frequency-map for favorable clinical outcome group showed that the lesions were concentrated at the right hemisphere, especially to the parietal to temporal lobe. This result indicates that favorable outcome is closely correlated with minor neurological symptoms even in cases with comparatively large ischemia as the lesions are located at non-functional brain. Furthermore, it became clear that ischemic volume after image standardization at the left hemisphere is correlated with clinical outcomes, and can be a useful predictive indicator. In addition, it was revealed that cerebral herniation was strongly influenced by ischemic volume after standardization 6,7.Acknowledgements
This research was supported by JSPS KAKENHI.References
1. Berkhemer, O. a. et al. A Randomized Trial of Intraarterial Treatment for Acute Ischemic Stroke. N. Engl. J. Med. 141217070022009 (2014). doi:10.1056/NEJMoa1411587
2. Takano, K. et al. Different spatial distributions of brain metastases from lung cancer by histological subtype and mutation status of epidermal growth factor receptor. Neuro. Oncol. 0, 1–9 (2015).
3. Amarenco, P., Bogousslavsky, J., Caplan, L. R., Donnan, G. A. & Hennerici, M. G. New approach to stroke subtyping: The A-S-C-O (phenotypic) classification of stroke. Cerebrovasc. Dis. 27, 502–508 (2009).
4. Kim, H. J. et al. Right-left propensity and lesion patterns between cardiogenic and aortogenic cerebral embolisms. Stroke 42, 2323–2325 (2011).
5. Carr, I. a, Nemoto, N., Schwartz, R. S. & Shadden, S. C. Size-dependent predilections of cardiogenic embolic transport. Am. J. Physiol. Heart Circ. Physiol. 305, H732-9 (2013).
6. Goto, Y. et al. Prediction of Malignant Middle Cerebral Artery Infarction in. J. Stroke Cerebrovasc. Dis. 25, 1389–1395 (2016).
7. Oppenheim, C. et al. Prediction of malignant middle cerebral artery infarction by diffusion-weighted imaging. Stroke. 31, 2175–2181 (2000).
Figures