4618
Evaluation of water permeability for ischemic lesion in the brain using DW-ASL1Hokkaido University Hospital, Sapporo, Japan
Synopsis
Diffusion-weighted arterial spin labeling technique was described to depict the tissue water permeability in the brain non-invasively; this information was also described to reflect the degree of blood-brain barrier damage. This study revealed that tissue water permeability can be useful for the evaluation of ischemic lesion more in detail than conventional technique such as T2WI or FLAIR for the determination of severity of ischemia and the prediction how fast the ischemia will progress.
Introduction
Water permeability from blood vessel to the tissue is one of important factor for the assessment of brain-blood barrier damage caused by numerous intracranial diseases including brain ischemia. Recently, non-invasive measurement of water permeability has been introduced by combining the arterial spin labeling and diffusion weighted imaging technique, called diffusion-weighted arterial spin labeling (DW-ASL) 1,2,3. The purpose of this study was to evaluate the water permeability in ischemic lesion of the brain using diffusion weighted arterial spin labeling method. The purpose of this study was to evaluate the water permeability in ischemic lesion of the brain using diffusion weighted arterial spin labeling (DW-ASL) method.Materials and Methods
1) Subjects and MR scanning
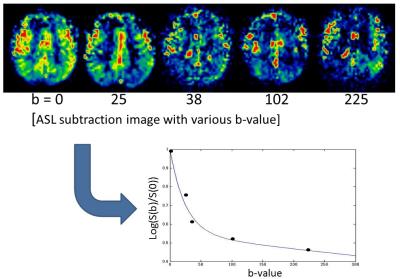
Eight patients (male; seven, female; one, age rage; 53-73, mean 61.5) with various degree of ischemic lesion in their brain were included. All patients were performed the MR scanning including T2WI, FLAIR, and DW-ASL. Five patients had the MR follow-up scanning history 3 years before DW-ASL scanning. All MR scanning was performed using 3-Tesla MR unit (Philips, Achieva TX) with 8-channel Head coil. ASL images were acquired by using pseudo-continuous labeling technique with the labeling duration of 1800 ms and post labeling delay of 1500 ms. Readout of 2D-EPI was used after the bipolar diffusion gradient in multiple b-values; total 5 scanning were performed using b-value of 0, 25, 38, 102 and 225 respectively.
2) Image analysis
2)-1 ROI placement
In each patient, whole brain was divided into 13 region of interest (ROI) based on the arterial dominant territory as follows; the bilateral flow territory of the anterior cerebral artery (ACA), middle cerebral artery (MCA) and posterior cerebral artery (PCA) on the upper level of lateral ventricle and level of basal ganglia, and cerebellum/pons.
2)-2 Determination of severity of ischemia and the presence of progression
In each segmented ROI in the brain of all patients, ischemic severity was divided into 3 groups (non-ischemic, moderate ischemic and severe ischemic lesion) based on the T2WI and FLAIR imaging findings. In addition, 5 patients with MR follow-up scanning history 3 years before DW-ASL scanning were also divided into two group (progressive and non-progressive ischemia group) based on the change of imaging findings between two scanning.
2)-3 Water permeability measurement
Water permeability was calculated from the signal intensity of ASL image in each b-value, using previously reported calculation method pixel by pixel basis as follows; 1) using the signal intensity of all 5 b-values, we calculated the capillary fraction by using past reported following bi-exponential function 1;
ΔM(b)/ΔM(0)=A1*e^(-b*D1)+A2*e^(-b*D2)
where ΔM(b) and ΔM(0) is the signal intensity of the subtraction image at the b-value denoted by the subscript and the b-value of 0, b is b-factor, A1 and A2 are the fraction of the fast (perfusion) and slow (tissue) component (A1 + A2 = 1), D1 and D2 are corresponding apparent diffusion coefficient. Next, 2) from the obtained value of capillary fraction A1, the water permeability value (Kw) was estimated the previously reported plot Graph which showed the relationship between capillary fraction and water permeability 2. The mean value of water permeability in each ROI was determined as each ROI’s water permeability value.
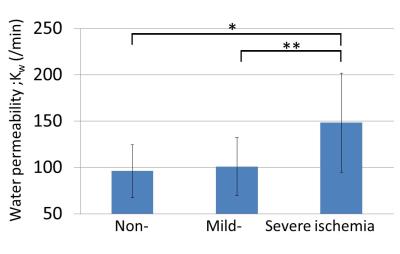
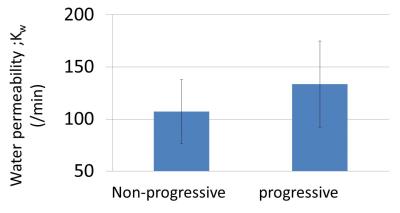
3) Statistical analysis
In all 102 ROIs in all 8 patients, the value of Kw was compared between ROIs based on the degree of ischemia (non-ischemia, mild ischemia and severe ischemia) by using ANOVA. Next, 65 ROIs in 5 patients with past follow-up MR examination, the value of Kw was compared between the ROIs based on the presence of progressive ischemia (progressive and non-progressive ischemia group) using the the Mann-Whitney U-test.
Results
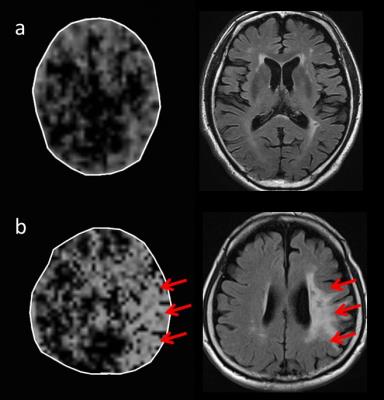
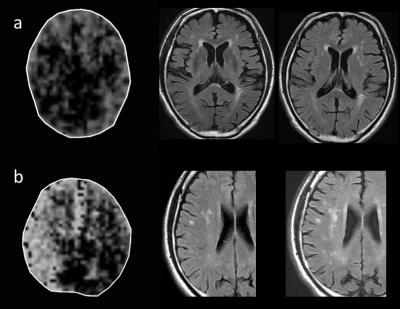
The Kw value in severe ischemia (148.3±53.2 min-1) was significantly higher than that of non-ischemia (96.3±28.6 min-1) and mild Ischemia (101.1±31.2 min-1) (p<0.05, respectively), in contrast, there was no significant difference between non-ischemia and mild ischemia (Fig. 2 and 3). The Kw value in progressive ischemia (133.5±41.3 min-1) was significantly higher than that of non-progressive ischemia (107.3±30.5 min-1) (p<0.05) (Fig. 4 and 5). In addition, increased permeability area tended to be visually larger than the ischemic lesion observed by T2WI and FLAIR (Fig. 3 and 5).Discussion and conclusion
The DW-ASL sequence was successfully performed. The water permeability obtained by DW-ASL can be an additional diagnostic tool for the evaluation of ischemic lesion in the brain as a new biological parameter. However, scanning time was too long. For the future perspective, scanning time will be shortened by combining other techniques such as multi-band acquisition or compressed sensing.Acknowledgements
No AcknowledgementsReferences
1. Wang J, Fernández-Seara MA, Wang S, et al. When perfusion meets diffusion: in vivo measurement of water permeability in human brain. J Cereb Blood Flow Metab. 2007;27(4):839-49.
2. St Lawrence KS, Owen D, Wang DJ. A two-stage approach for measuring vascular water exchange and arterial transit time by diffusion-weighted perfusion MRI. Magn Reson Med. 2012;67(5):1275-84.
3. Tiwari YV, Lu J, Shen Q, et al. Magnetic resonance imaging of blood-brain barrier permeability in ischemic stroke using diffusion-weighted arterial spin labeling in rats. J Cereb Blood Flow Metab. 2016 Oct 14 [Epub ahead of print]
Figures