4614
A quantitative analysis using susceptibility mapping of unilateral middle cerebral artery thrombosis in patients with acute cerebral infarction1Tianjin First Central Hospital, Tianjin, People's Republic of China, 2Radiology Department, Tianjin First Central Hospital, Tianjin, People's Republic of China
Synopsis
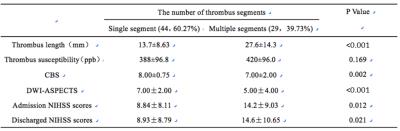
The aim of this study was to explore the correlation between thrombus length, thrombus susceptibility, CBS, DWI-ASPECTS, and admission and discharge NIHSS scores between patients with single-segment and multiple-segment thrombi using susceptibility mapping (SWIM). SWIM, reconstructed from magnitude and phase images acquired by an SWI sequence, was used to measure thrombus susceptibility in patients with acute infarction. A higher susceptibility of thrombus was correlated with lower DWI-ASPECTS and increased NIHSS scores. The patients with multiple-segment thrombi had a larger area of cerebral infarction, more severe symptoms, and worse clinical outcomes.
PURPOSE
Arterial thrombosis is the most common cause of acute cerebral infarction1. Early detection and accurate evaluation of the thrombus plays an important role in treatment planning and predicting clinical outcome. Although digital subtraction angiography (DSA) and computed tomography angiography (CTA) are useful for imaging thrombi, they are invasive. Additionally, time-of-flight magnetic resonance angiography (TOF-MRA) has been used; however, it had a poor resolution. It has been reported that the sensitivity of susceptibility-weighted imaging (SWI) in the detection of cerebral thrombosis is higher than that of DSA and TOF-MRA1, 2. Recently, susceptibility-weighted image and mapping (SWIM) used for the quantitative measurement of thrombus susceptibility was introduced3. To date, there has been no quantitative study investigating the thrombosis susceptibility and the effect of thrombus burden factors on cerebral infarction. In our study, we aimed to explore the correlation between thrombus, clot burden scores (CBS), DWI-Alberta stroke program early CT scores (DWI-ASPECTS), and the admission and discharge National Institute of Health Stroke Scale (NIHSS) scores between patients with a single segment of thrombus and with multiple segments of thrombi.Methods
A total of 73 patients was included in this retrospective study. The inclusion criteria was: 1) 18 years of age or older; 2) middle cerebral artery territory showing hyperintensity on DWI and hypointensity on ADC; 3) patient had unilateral MCA occlusion confirmed by TOF-MRA and corresponding thrombosis confirmed by SWI; 4) patient had no other diseases and had not undergone neurosurgery. The patients were divided into two groups: those with a single segment of thrombus (44 patients) and multiple segments of thrombi (29 patients) based on the number of thrombi segments on SWI. MRI data were collected on a MAGNETOM Trio Tim 3T MR scanner (Siemens, Erlangen, Germany) including a routine head scan and SWI. The parameters of SWI were: TR/TE=27/20ms; field of view=230×200mm2; receiver bandwidth=120 Hz/pixel; flip angle=15°; number of slices=56; acquisition time=179s; voxel size=0.5×0.5×2mm³. SWIM was reconstructed using both the phase and magnitude data using SMART (Susceptibility Mapping and Phase Artifacts Removal Toolbox, Detroit, Michigan, USA) software. The length and susceptibility of thrombus were measured using SPIN (Signal Processing in Nuclear Magnetic Resonance, Detroit, Michigan, USA) software (Fig. 1). The thrombus segment (single or multiple segments), length, susceptibility, and CBS were also recorded. DWI-ASPECTS was measured to estimate the cerebral infarction region. The admission and discharged NIHSS scores were assessed by a neurologist with 13 years of experience. The correlation analyses were used to explore the correlation between thrombus length, thrombus susceptibility, CBS, DWI-ASPECTS, and admission and discharge NIHSS scores. Independent-sample t-tests and Mann-Whitney U analyses were used to explore the difference between the single-thrombus segment group and the multiple-segments group.Results
The MCA thrombus length negatively correlated with DWI-ASPECTS (r=-0.492, P<0.001) and CBS (r=-0.401, P<0.001) and positively correlated with admission NIHSS scores (r=0.283, P=0.015) (Fig. 2). The thrombus susceptibility positively correlated with admission NIHSS scores (r=0.241, P=0.040) and discharge NIHSS scores (r=0.330, P=0.004), and negatively correlated with DWI-ASPECTS (r=-0.248, P=0.034) (Fig. 3). The CBS positively correlated with DWI-ASPECTS (r=0.349, P=0.002) and negatively correlated with admission and discharge NIHSS scores (r=-0.318, P=0.006; r=-0.274, P=0.019) (Fig. 4). The CBS and DWI-ASPECTS in the multiple-segments group were significantly lower than that in the single-segment group (P=0.002, P<0.001, respectively). The thrombus length and admission and discharge NIHSS scores in the multiple-segments group were significantly higher than that in the single-segment group (P<0.001, P=0.012, P=0.021) (Table 1).Discussion
In our study, we found that the MCA thrombus length negatively correlated with DWI-ASPECTS and CBS and positively correlated with admission NIHSS scores. It has been reported that lower DWI-ASPECTS and CBS indicate a larger size of cerebral infarction because a longer thrombus can cause an increased infarction area. 4,5 More severe cerebral infarctions result in increased admission NIHSS scores. We also found that MCA thrombus susceptibility positively correlated with admission and discharge NIHSS scores and negatively correlated with DWI-ASPECTS. The higher-susceptibility thrombus had more deoxyhemoglobin, indicating that the thrombus was in an acute stage. After the acute stage, the cerebral tissues exhibited tissue repair so that symptoms were reduced and the area of cerebral infarction became gradually smaller. Therefore, acute thrombus can cause more severe symptoms reflected in the increased NHISS scores and a larger infarction region, which negatively correlated with DWI-ASPECTS.Conclusion
A high susceptibility value of thrombus can indicate low DWI-ASPECTS and increased NIHSS scores. The CBS could be an index of increased DWI-ASPECTS and decreased NIHSS scores. The patients with multiple-segment thrombi had a larger size of cerebral infarction, more severe symptoms, and worse clinical outcome.Acknowledgements
The contribution of each author to the work was listed as followed: Shuang Xia (S.X.): substantial contributions to conception and design; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; Chao Chai (C.C.): substantial contributions to conception and design, acquisition of data, or statistical analysis and interpretation of data; Qingyuan Yang (Q.Y.Y.): contributions to conception and design; acquisition of data, or analysis and interpretation of data; Tianyi Qian (T.Y.Q.): analysis and interpretation of data; E Mark Haacke (E.M.H.): substantial contributions to conception and design; analysis and interpretation of data; revising it critically for important intellectual content; Wen Shen (W.S.): substantial contributions to conception and design.References
[1] Radbruch. A, Mucke. J, Schweser. F, et al. Comparison of Susceptibility Weighted Imaging and TOF-Angiography for the Detection of Thrombi in Acute Stroke [J]. PLoS One, 2013, 8(5): e63459.
[2] Lingegowda D, Thomas B, Vaghela V, et al. 'Susceptibility sign' on susceptibility-weighted imaging in acute ischemic stroke [J]. Neurol India, 2012, 60(2): 160-164.
[3] Haacke EM, Tang J, Neelavalli J, Cheng YC. Susceptibility mapping as a means to visualize veins and quantify oxygen saturation. J MagnReson Imaging. 2010 Sep;32(3):663-76.
[4] de Margerie-Mellon C, Turc G, Tisserand M, et al. Can DWI-ASPECTS substitute for lesion volume in acute stroke? [J]. Stroke, 2013, 44(12): 3565-3567.
[5] Legrand L, Naggara O, Turc G, et al. Clot burden score on admission T2*-MRI predicts recanalization in acute stroke [J]. Stroke, 2013, 44(7): 1878-1884.
[6] Gratz PP, Schroth G, Gralla J, et al. Whole-Brain Susceptibility-Weighted Thrombus Imaging in Stroke: Fragmented Thrombi Predict Worse Outcome [J]. Am J Neuroradiol, 2015, 36(7): 1277-1282.
Figures

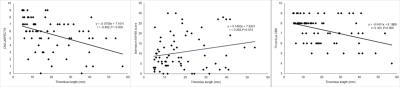
Fig. 2 The correlation between thrombus length and CBS, DWI-ASPECTS, and admission NIHSS scores.
The MCA thrombus length negatively correlated with DWI-ASPECTS (r=-0.492, P<0.001) and CBS (r=-0.401, P<0.001), and positively correlated with admission NIHSS scores (r=0.283, P=0.015).
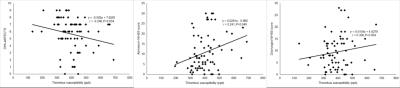
Fig. 3 The correlation between thrombus susceptibility and DWI-ASPECTS, admission and discharge NIHSS scores.
The MCA thrombus susceptibility value positively correlated with admission NIHSS scores (r=0.241, P=0.040) and discharge NIHSS scores (r=0.330, P=0.004) and negatively correlated with DWI-ASPECTS (r=-0.248, P=0.034).
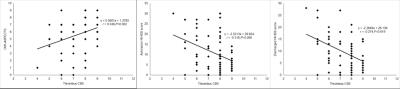
Fig. 4 The correlation between CBS, DWI-ASPECTS, admission and discharge NIHSS scores.
The CBS values positively correlated with DWI-ASPECTS (r=0.349, P=0.002) and negatively correlated with admission and discharge NIHSS scores (r=-0.318, P=0.006;r=-0.274, P=0.019).