4574
The use of Arterial Spin Labeling to Evaluate Posterior Circulation Ischemia in the elderly group (>80 years)1Department of Radiology, General Hospital of the People’s Liberation Army, Beijing, People's Republic of China, 2General Hospital of the People’s Liberation Army, 3GE Healthcare company
Synopsis
Contrast free arterial spin labeling approach is used to assess the perfusion changes in PCI in the elderly group (>80yrs)compared with normal control elderly group. Lower perfusion level was seen in PCI group, also a long PLD time is more effective in detecting the PCI group in case of slower perfusion rate. The lower level of increment with a long PLD in PCI group also indicates the weakened perfusion ability in the posterior circulation.
Purpose
The attention on elderly ischemic stroke was mainly focused on anterior circulation ischemia. On the other hand, although accounts for 20% of the elderly ischemic stroke, due to the lack of typical symptoms and diagnostic criteria, posterior circulation ischemia is being less studied[1]. Pathologically, it is a clinical syndrome of focal hypo cerebral blood perfusion caused by vessels stenosis, in situ thrombosis or embolism in posterior circulation region. CT perfusion that reflects the cerebral perfusion level has been used for detecting PCI[2, 3]. However, for the elderly group beyond 80 years old, they suffer high risk of exogenous agent and is banned from the use of contrast in medical centers. Hence imaging study for PCI in elderly group beyond 80 years old is lacking. In this study, we investigate the use of contrast free arterial spin labeling approach to assess the perfusion changes in PCI in the elderly group.Method
A total of 53 subjects older than 80 years were recruited for this ethic committee approved study and consent forms were obtained prior to the scans. Patient group included 20 subjects (n=20;20 males; age=85.53±9.28) who showed PCI symptoms including dizziness, headache, diplopia, visual impairment, etc. and excluded benign paroxysmal vertigo by Dix-Hallpike examination as well as cervical vertigo by X-ray and transcranial Doppler (TCD). Other 33 (n=33;33 males; age=84.14±6.7) who were asymptomatic were recruited as the healthy control. All subjects underwent 3D arterial spin labeling as well as clinical routine scans (T1, T2 and DWI). Two post labeling delay (PLD) times were used (PLD = 1.5s, 2.5s). A high-resolution volumetric IR prepped T1W sequence was used to for anatomical registration, which was then registered to a standardized space (MNI template)[4, 5]. All quantitative CBF maps were normalized to the MNI space. Standard anatomical regions of interests (ROIs) were identified. Mean cerebral blood flow (CBF)values of every encephalic region of the cortex of bilateral occipital lobes and bilateral cerebellums were measured. Independent sample t-test and rank-sum test were performed to evaluate (1) the difference of CBF changes of anterior circulation and posterior circulation in two groups of two PLDs;(2) the difference of CBF changes of bilateral occipital lobes and bilateral cerebellums in two groups of two PLD time; (3) the difference of increment of CBF between two PLD interval between two groups. If the data conformed to normal distribution, two independent samples T test was adopted; if not, rank-sum test was adopted. P<0.05 was regarded as the statistical significance threshold in the present study.Results
The CBF maps of a normal control and a PCI patient with both PLDs are shown in Fig. 1 and 2 respectively. Table 1and 2 respectively shows the comparation between CBF values of anterior circulation and posterior circulation as well as bilateral occipital lobes and bilateral cerebellums in patient group and control group of different PLD time. Table 3 shows comparation between CBF increment values of bilateral occipital lobes and bilateral cerebellums in patient group and control group. The PCI patient showed a visually lower perfusion level in comparison to the healthy control. Comparing to control group, significantly lower CBF was observed in bilateral occipital lobes and bilateral cerebellums. The measured CBF showed significant significance in anterior and posterior circulation for the patient group in both PLDs, whereas such difference was only observed in PLD = 1.5s in the control group. In addition, the increment of CBF with a prolonged PLD was significantly lower in the PCI group as compared to the control group.Discussion and conclusion
In this work, the use of multiple PLD ASL for the detection of PCI in subjects older than 80 group was investigated. This study attempts to address the clinical need that PCI lacks clinical diagnosis criteria and the elderly group (>80 yrs.) cannot receive exogenous contrast. It was seen that ASL was able to reveal the lower perfusion level in PCI group, also that a long PLD time is more effective in detecting the PCI group in case of slower perfusion rate. The lower level of increment with a long PLD in PCI group also indicates the weakened perfusion ability in the posterior circulation. Hence ASL may be a viable and non-invasive approach for detecting PCI in elderly group.Acknowledgements
We thanked Weiwei Men,Phd,at MRI research centre of Peking University and Bing Wu,Phd and Nan Xie,Phd,at GE Healthcare,Beijing,China,for excellent technical assistance.References
$$ 1.Markus, H.S., H.B. van der Worp, and P.M. Rothwell, Posterior circulation ischaemic stroke and transient ischaemic attack: diagnosis, investigation, and secondary prevention. The Lancet Neurology, 2013. 12(10): p. 989-998.
$$ 2.Schulz, U.G. and U. Fischer, Posterior circulation cerebrovascular syndromes: diagnosis and management. J Neurol Neurosurg Psychiatry, 2016.
$$3.Merwick, A. and D. Werring, Posterior circulation ischaemic stroke. BMJ, 2014. 348: p. g3175.
$$4.Maldjian, J.A., et al., An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage, 2003. 19(3): p. 1233-9.
$$5.Lancaster, J.L., et al., Automated Talairach atlas labels for functional brain mapping. Hum Brain Mapp, 2000. 10(3): p. 120-31.
Figures
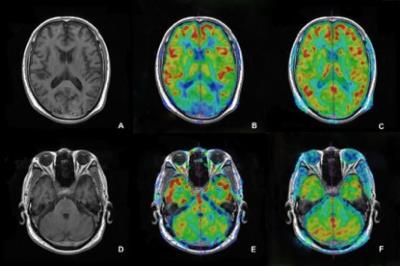
Fig1 CBF image of posterior circulation in different PLD time of normal elder subject
A.3D FSPGR T1WI anatomic image of occipital lobe; B. hypo perfusion of bilateral occipital lobe in the image of CBF (PLD=1525ms); C. hypo perfusion of bilateral occipital lobe disappeared in the image of CBF (PLD=2525ms); D. 3D FSPGR T1WI anatomic image of cerebellum; E. image of CBF (PLD=1525ms); F. image of CBF (PLD=2525ms)
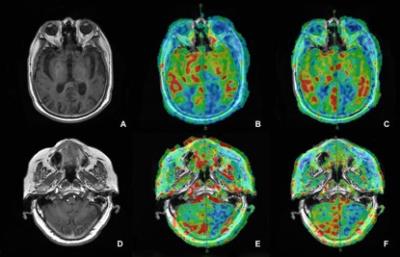
Fig2 CBF image of posterior circulation in different PLD time of elder PCI subject
This is a 93-year old male patient, who had a complaint about dizziness with blurring of vision, weakness of bilateral lower limbs and deglutition barrier. He was diagnosed as PCI by the clinic.
A.3D FSPGR T1WI anatomic image of occipital lobe; B. hypo perfusion of bilateral occipital lobe(especially left side)in the image (PLD=1525ms); C. hypo perfusion in the image (PLD=2525ms); D. 3D FSPGR T1WI anatomic image of cerebellum; E. hypo perfusion of left side in the image(PLD=1525ms); F. hypo perfusion of left side in the image(PLD=2525ms)
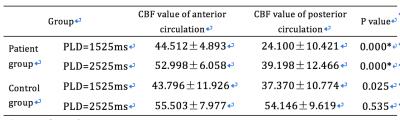
Table 1 Comparation between CBF values of anterior circulation and posterior circulation in patient group and control group of different PLD time(`x±s,ml·100g-1·min-1)
*present for rank-sum test.
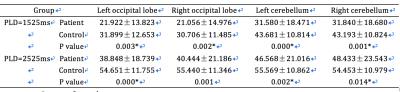
Table 2 Comparation between CBF values of bilateral occipital lobes and bilateral cerebellums in patient group and control group of different PLD time(`x±s,ml·100g-1·min-1)
*present for rank-sum test.
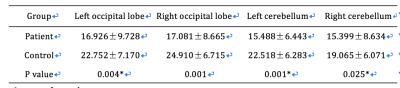
Table 3 Comparation between △CBF values of bilateral occipital lobes and bilateral cerebellums in patient group and control group(`x±s,ml·100g-1·min-1)
*present for rank-sum test.