4571
4D Flow assessment of ophthalmic artery flow in patients with atherosclerotic internal carotid artery stenotic disease1Radiology, Nippon Medical School, Tokyo, Japan, 2Radiology, Nihon University School of Medicine, Tokyo, Japan, 3Neurosurgery, Nippon Medical School, Tokyo, Japan
Synopsis
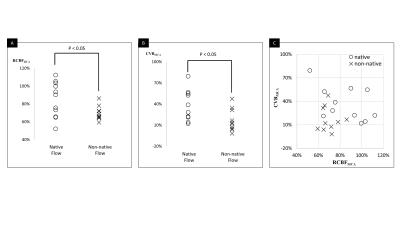
We performed 4D Flow MRI assessment of the ophthalmic artery (OphA) flow in patients with internal carotid artery stenosis (ICS). Twenty-one consecutive patients with unilateral ICS were recruited. 4D Flow MRI and acetazolamide-stress brain perfusion SPECT were performed. The flow direction on the affected-side OphA was categorized into native flow and non-native flow based on 4D Flow MRI. In the affected-side MCA territory, the ratio of rest cerebral blood flow to normal control (RCBFMCA) and cerebral vascular reserve (CVRMCA) were calculated from SPECT dataset. Eleven patients had native OphA flow and the remaining 10 had non-native OphA flow. RCBFMCA and CVRMCA were significantly lower in non-native flow group (84.9±18.9% vs. 69.8±7.3%, p<0.05; 36.4±20.6% vs. 17.0±15.0%, p<0.05). Four patients in the non-native flow group and none in the native flow group were confirmed as high-risk (Sensitivity/Specificity, 1.00/0.65). The 6 min-standard 4D Flow MRI assessment of OphA in patients with ICS can predict intracranial hemodynamic impairment.
Introduction
Internal carotid artery stenotic disease (ICS) is a common condition in patients with atherosclerosis and considered a risk factor for transient ischemic disease (TIA) or cerebral infarction (CI). The prognosis of patients with ICS correlates not only with the severity of stenosis itself but also with how the collateral pathway compensates for the decrease in blood flow from the internal carotid artery (ICA). Among these collateral pathways, the retrograde flow through the affected-side ophthalmic artery (OphA) has been considered a sign of inadequate circulation because it reflects the reduction of arterial pressure in the distal ICA [1].
The purposes of this study was to assess the feasibility of (Time-resolved 3D phase contrast) 4D Flow MRI assessment of OphA flow in ICS patients by comparing with single photon emission CT (SPECT) data combined with acetazolamide challenge.
Matrials and Methods
Twenty-one consecutive patients with unilateral ICS were recruited. 4D Flow MRI and acetazolamide-stress brain perfusion SPECT were performed. 4D Flow MRI was performed using a 3.0-T MRI unit (Achieva; Philips Healthcare, Best, The Netherlands). The 4D Flow MRI parameters were as follows: repetition time/echo time (TR/TE) 8.4/5.4 ms; k-space segmentation factor 2; temporal resolution 67.2 ms; flip angle (FA) 13°; velocity encoding (VENC) 70 cm/s (VENC range, 140cm/sec), voxel size 0.82×0.82×1.4 mm3; 15 cardiac phases; sensitivity encoding (SENSE) factor 2; elliptical partial k-space coverage in phase- and slice-encoding direction; and acquisition time 6 min. The flow direction on the affected-side OphA was categorized into native flow (anterograde or unclear) and non-native flow (retrograde flow) based on 4D Flow MRI. In the affected-side MCA territory, the ratio of rest cerebral blood flow to normal control (RCBFMCA) and cerebral vascular reserve (CVRMCA) were calculated from SPECT dataset. To assess the severity of hemodynamic impairment, we compared the cerebral perfusion, RCBFMCA or CVRMCA data between two patient groups by using Student’s t-test. These quantitative value relates to the risk for stroke recurrence in patients with ICS [2].High-risk patients were defined based on the previous large cohort study (RCBFMCA < 80% and CVRMCA < 10%) [2].
Results
Eleven patients had native OphA flow and the remaining 10 had non-native OphA flow. RCBFMCA and CVRMCA each were significantly lower in non-native flow group (84.9±18.9% vs. 69.8±7.3%, p<0.05; 36.4±20.6% vs. 17.0±15.0%, p<0.05). Four patients in the non-native flow group and none in the native flow group were confirmed as high-risk (Sensitivity/Specificity, 1.00/0.65).Discussion
4D Flow MRI features several advantages for the assessment of the OphA, as described below. First, compared with angiography or ultrasound imaging, the 4D Flow sequence can be easily combined with a clinical MRI workup. In the patients with ICS, follow-up is mainly performed using MRI because it is non-invasive and one of the most objective methods. In addition, 4D Flow MRI can be widely performed using a clinical scanner. Second, compared with 2D phase-contrast imaging, one of the advantages of 4D Flow is that it can acquire comprehensive flow information in a large FOV, which allows operators to save the procedure for selecting the imaging slice perpendicular to the target vessel. If the target vessel, OphA, is small or complex, the examination requires a highly skilled operator during the MRI scan, which is difficult in a clinical setting. Third, 3D spatial information with three directions of velocity information enables to reconstruct oblique plane along to the OphA which improves the visualization of the flow in the small vessel. As shown in the figures in this study, the vector map helps the investigators intuitively recognize the flow direction of OphA.
The limitations of our study are described below. First, the patient population was small. However, the quantitative value related to the hemodynamic impairment was significantly different between patients groups. Second, we defined impairment of cerebral perfusion using the SPECT data, not clinical outcome. The correct assessment of clinical outcome was difficult in our small sample, which featured various medication and/or surgical treatments. However, previous studies have proved CBF and CVR can correctly predict the risk of the recurrent stroke [2]. Third, only one neuroradiologist evaluated the 4D Flow MRI. Nevertheless, previous 4D Flow studies have proven high inter-observer agreement.
Conclusion
The standard 4D Flow MRI with a 6 min scan can assess the flow in the ophthalmic artery. This assessment can predict the subsequent prognosis of the patients with internal carotid artery stenosis.Acknowledgements
None.References
(1) Tsai CL, Lee JT, Cheng CA, et al. Reversal of ophthalmic artery flow as a predictor of intracranial hemodynamic compromise: implication for prognosis of severe carotid stenosis. Eur J Neurol 2013;20:564-570.
(2) Kataoka H, Miyamoto S, Ogasawara K, et al. Results of Prospective Cohort Study on Symptomatic Cerebrovascular Occlusive Disease Showing Mild Hemodynamic Compromise [Japanese Extracranial-Intracranial Bypass Trial (JET)-2 Study]. Neurol Med Chir (Tokyo) 2015;55:460-468.
Figures