4569
Prevalence and Clinical Relevance of Intraplaque Haemorrhage in Stenotic and Non-stenotic Basilar Artery Intracranial Atherosclerotic Plaque1Radiology, University of California, San Francisco, San Francisco, CA, United States, 2Radiology, Changhai Hospital, Shanghai, People's Republic of China, 3Radiology, University of Pittsburgh, PA, United States, 4Radiology, University of Cambridge, Cambridge, United Kingdom
Synopsis
Intraplaque hemorrhage (IPH) in intracranial arteries is a possible marker of increased stroke risk. While previous studies focused on stenotic arteries, non-stenotic arteries also cause fatal stroke. We studied 100 patients using high-resolution MRI and found IPH was prevalent (>20%) in both stenotic and non-stenotic basilar arteries, and was a strong predictor of symptoms with an odd ratios of 15.4. IPH has a very high specificity (97.1%) to predict symptoms. Specifically, IPH may be useful in selecting high risk stroke patients with clinically non-significant stenosis, who may benefit from more aggressive treatment.
Purpose
Intracranial atherosclerotic disease (ICAD) is a major cause of stroke that has been underappreciated, in part due to challenges in detecting intracranial atherosclerotic plaque 1. With the development of high resolution black blood MRI (hrMRI) techniques, intracranial vessel wall characteristics such as fresh intraplaque hemorrhage (IPH) have been increasingly studied as possible markers of neurological symptoms2. However, previous studies of intracranial IPH focused on stenotic arteries (degree of stenosis >50%)3 4, while it is known that non-stenotic (<50% stenosis) atherosclerotic plaque can also cause fatal stroke 5. This study aims to study the prevalence and clinical relevance of IPH in patients with stenotic and non-stenotic (<50%) basilar artery plaques.Methods
Study Population: 100 patients (74 male, age 61±10) with cerebral ischemic events were recruited and were divided into three groups based on their symptom presentation: 1) Acute symptomatic if symptoms were present within 4 weeks; 2) Sub-acute symptomatic if within 4-12 weeks; 3) Asymptomatic/chronic if more than 12 weeks. Image acquisition: MR images were acquired on a Siemens 3T scanner using standard head-neck coils. HrMRI of basilar plaque included 3D TOF and black blood sequences: pre- and post-Gd contrast T1-weighted fast spin echo (FSE) and T2-weighted FSE. TR/TEs for T1 and T2 weighted FSE: 800ms/13ms and 2880ms/53ms. An in-plane resolution of 0.4mm and a slice thickness of 2mm were used. Clinical brain imaging included T1/T2-weighted FSE, FLAIR and DWI. Image Analysis: Presence of fresh IPH was identified as >150% signal of nearby auricularis anterior muscles on pre-contrast T1-weighted images4 by two blinded reviewers. Plaque burden (PB) was defined as (1 – Lumen Area/Outer Area)x100%. The relationship between image findings (IPH, contrast enhancement, degree of stenosis, minimal lumen area [MLA] and PB) and symptoms were analysed.Results
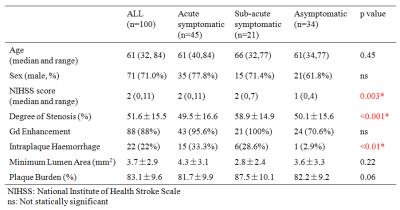
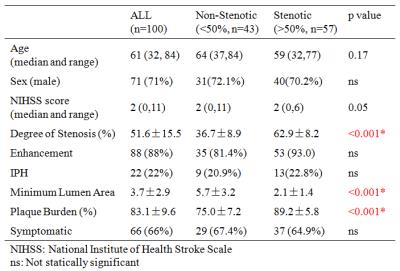
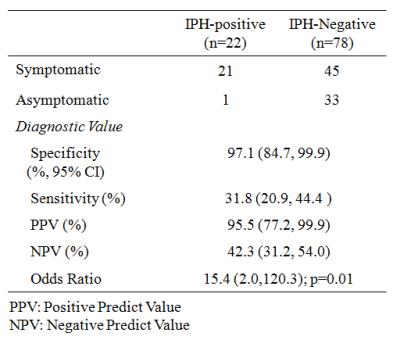
An example of IPH in a patient with recent post-circulation stroke is shown in Figure 1. There was an excellent inter-reader agreement for identifying IPH (96% agreement, Cohen’s κ=0.88) and quantifying degree of stenosis (r=0.97). IPH was identified in 22 patients (22%), including 15 (33.3%) acute patients, 6 (28.6%) sub-acute patients, and 1 (2.9%) asymptomatic patient (Table 1). IPH was the strongest predictor of symptomatic status (odds ratio [95% confidence interval]: 15.4 [2.0,120.3]; p=0.01). Contrast enhancement, stenosis, MLA and PB were not correlated with symptoms (p>0.05). IPH appeared over a range of stenosis values (Table 2), and there was no difference in the prevalence rate in stenotic and non-stenotic basilar arteries (20.9% vs. 22.8%, p>0.05). IPH was a strong predictor of symptoms, regardless of the stenosis values. Diagnostic performance of IPH for symptomatic stroke patients is summarized in Table 3. IPH had a high specificity of 97.1% and high positive predictive value of 95.5%, however its sensitivity and negative predictive value were lower than 50%.Discussion
To the best of our knowledge, this is the first study to report IPH prevalence and its clinical relevance in non-stenotic intracranial arteries. We found IPH to be a strong predictor of symptom presentation with an odds ratio >15, and the prediction power is maintained regardless the degree of stenosis. Current practice guidelines rely solely on the degree of stenosis (often ≥ 50%) within major intracranial arteries to direct management, but many authors have called this practice into question, especially given the high prevalence of mild and moderate intracranial arterial stenosis in fatal stroke as found at autopsy 5. Interestingly, we found the prevalence of IPH is similar in stenotic and non-stenotic basilar arteries. Our results suggest that IPH can be used to select high risk patients in the non-stenotic group, who may benefit from more aggressive treatment. Although high specificity and low sensitivity indicates that a patient with IPH is very likely at high risk, the absence of IPH does not imply low risk. This may suggest that IPH is only one of many mechanisms causing plaque vulnerability. Our reported prevalence rate is lower than has previously been published (42.3%) 4, possibly because our patient cohort has less severe symptoms (low NIHSS scores) and is much younger (61yrs vs. 72.5yrs). In addition, IPH can be reliably detected by T1 weighted hrMRI as demonstrated by excellent inter-reader agreement, which makes it a promising tool for clinical use. The prognostic value of intracranial IPH in predicting stroke should be evaluated in larger scale, prospective studies.Conclusion
IPH is prevalent in both stenotic and non-stenotic basilar artery plaque, and is associated with stroke symptoms. IPH provides new insights in the management of stroke patients with clinically non-significant stenosis.Acknowledgements
This study was supported by the Twelfth Five Year Plan Medical Key Project of the People's Liberation Army, China (BWS12J026),Shanghai Hospital Development Center grant (SHDC12013110), andthe National Natural Science Foundation of China (NSFC)(31470910).References
1. Gorelick, P. B., Wong, K. S., Bae, H. J. & Pandey, D. K. Large artery intracranial occlusive disease: a large worldwide burden but a relatively neglected frontier. Stroke 39, 2396-2399, (2008).
2. Dieleman, N. et al. Imaging intracranial vessel wall pathology with magnetic resonance imaging: current prospects and future directions. Circulation 130, 192-201, (2014).
3. Xu, W. H. et al. Middle cerebral artery intraplaque hemorrhage: prevalence and clinical relevance. Ann Neurol 71, 195-198, (2012).
4. Yu, J. H. et al. Association of Intraplaque Hemorrhage and Acute Infarction in Patients With Basilar Artery Plaque. Stroke 46, 2768-2772, (2015).
5. Mazighi, M. et al. Autopsy prevalence of intracranial atherosclerosis in patients with fatal stroke. Stroke 39, 1142-1147, (2008).
Figures