4568
Association between Occluded Extra-cranial Carotid Artery Disease and Arterial Wall Edema in Ipsilateral Petrous Internal Carotid Artery: A 3D MR Vessel Wall Imaging Study1Beijing Institute for Brain Disorders, Capital Medical University, Beijing, People's Republic of China, 2Center for Biomedical Imaging Research, Department of Biomedical Engineering, Tsinghua University, Beijing, People's Republic of China, 3Department of Radiology, Renji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, People's Republic of China, 4Philips Research China, Philips Healthcare, Beijing, People's Republic of China, 5Department of Radiology, University of Washington, Seattle, United States
Synopsis
Carotid artery severe stenosis or occlusion will lead to decreases in blood flow and ischemia in downstream arterial segments. It has been shown that ischemia within vessel wall may lead to wall edema which will affect the vascular revascularization after interventional treatment for the severe stenotic or occluded diseases. This study investigated the correlation between extra-cranial carotid artery stenotic diseases and arterial wall edema in ipsilateral petrous internal carotid artery (ICA) using 3D MR vessel wall imaging. We found that proximal ICA severe stenosis was independently associated with wall edema in ispilateral petrous ICA (OR=2.45, 95% CI 1.65-3.63, P<0.001).
Introduction
Carotid artery severe stenosis or occlusion will lead to decreases in blood flow of downstream arterial segments and subsequently ischemia.[1,2] The ischemia within the vessel wall may activate the inflammation process and then lead to wall edema. The severe wall edema might affect the vascular revascularization during interventional treatment for the severe stenotic or occluded diseases. Therefore, it is important to find an effective surrogate for arterial wall edema prior to revascularization treatment. The phenomenon of vessel wall edema has been successfully detected by 2D T2-weighted (T2W) short-tau inversion recovery (T2-STIR). [3,4] Recently, 3D vessel wall imaging techniques, such as Motion Sensitized Driven Equilibrium prepared Rapid Gradient Echo (MERGE), has been proposed to evaluate the vessel wall diseases in more vascular segments than 2D imaging techniques due to its large longitudinal coverage. [5] The 3D MERGE used the iMSDE prepulse [6] to suppress the flowing spins. Since iMSDE was applied as a black blood preparation module in 3D MERGE, there is substantial T2 weighting.Purpose
This study sought to investigate the correlation between occluded extra-cranial carotid artery diseases and arterial wall edema in the ipsilateral petrous internal carotid artery using 3D MR vessel wall imaging.Methods
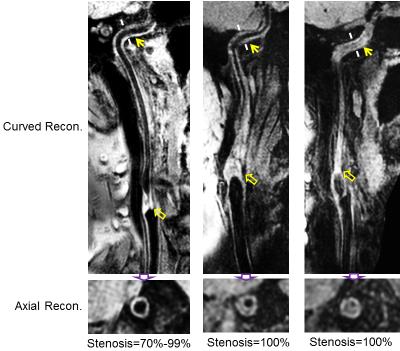
Study sample: Patients with cerebrovascular symptoms and severe carotid stenotic atherosclerotic disease (≥50% stenosis) were recruited in this study. MR imaging: All subjects underwent carotid MR vessel wall imaging on a 3.0 T Philips MR scanner with 8-channel carotid coil. The 3D MERGE sequence was acquired with the following parameters: fast field echo sequence, repeat time/echo time 9.2/4.3 ms, flip angle 6°, field of view 40×160×150 mm3, resolution 0.8×0.8×0.8 mm3. A 3D TOF MRA was acquired for stenosis measurement. Carotid arteries with poor image quality and dissection were excluded. Data analysis: Two radiologists interpreted the MR images with consensus. The degree of stenosis of proximal internal carotid artery (ICA) was measured and classified into the following categories: 50%-69%, 70%-99% and 100% (total occlusion). The vessel wall edema in petrous ICA was defined as diffuse wall thickening with iso- to hyperintense on MERGE images but isointense on TOF images. The severity of wall edema was divided into 2 categories: mild edema, thickness <2mm; and severe edema, thickness ≥2mm. The prevalence of wall edema in different stenosis categories was calculated. The correlation between edema in petrous ICA and proximal ICA stenosis was determined.Results
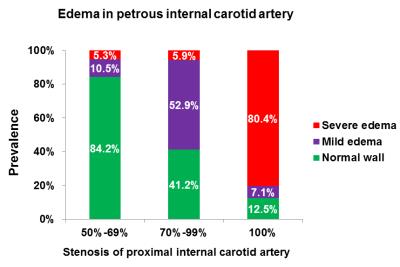
In total, 92 carotid arteries (89 patients, mean age 60.9±12.1 years, 77 males) with acceptable image quality were included in the final analysis. Of all 92 carotid arteries, 19 had 50%-69% stenosis, 17 had 70%-99% stenosis, and 56 had total occlusion in proximal ICA and 62 (67.4%) had wall edema in petrous ICA. The distribution of wall edema in petrous ICA in different categories of carotid stenosis in proximal ICA was detailed in Figure 1. Severe edema in petrous ICA was common (80.4%) in ipsilateral carotid arteries with total occlusion in proximal ICA. Spearman’s correlation analysis revealed that the stenosis degree of proximal ICA was significantly correlated with wall edema in petrous ICA (r=0.60, P<0.001). Logistic regression analysis showed that the odds ratio (OR) of the proximal ICA stenosis with increment of 10% was 2.41 (95% confidence interval [CI]: 1.71-3.40, P<0.001) in discriminating presence of wall edema in petrous ICA. After adjusted for confounding factors, this association was still significant (OR=2.45, 95% CI 1.65-3.63, P<0.001). The examples for carotid arteries with severe stenosis in proximal ICA having wall edema in ipsilateral petrous ICA are presented in Figure 2.Discussion
We found that severe stenosis in proximal ICA was significantly associated with wall edema in ispilateral petrous ICA. To the best of our knowledge, this study is one of the first to report the phenomenon that wall edema in downstream arterial segment due to severe stenotic disease in proximal ICA. The phenomenon of wall edema can be explained by the mechanism of ischemia. The sequelae of wall edema are unclear. This study utilized MERGE sequence with both T1W and T2W components to characterize the wall edema. Future studies are warranted to use 3D fast spin echo T2W imaging techniques to visualize this pathology. In addition, carotid coil was used to receive the MR signal in this study but it has limited coverage and signal to noise ratio, particular for the area of petrous segment of ICA. Neurovascular coil with large coverage is suggested to use in future studies.Conclusion
Severe stenotic disease in proximal internal carotid artery is associated with the arterial wall edema in the ipsilateral petrous segment of internal carotid artery.Acknowledgements
None.References
1. Gibbs JM, Wise RJS, Leenders KL, et al. Evaluation of cerebral perfusion reserve in patients with carotid-artery occlusion. Lancet. 1984;1(8372):310-4.
2. Powers WJ, Press GA, Grubb RL Jr, et al. The effect of hemodynamically significant carotid artery disease on the hemodynamic status of the cerebral circulation. Ann Intern Med. 1987;106:27-34.
3. Pedersen SF, Kim WY, Paaske WP, et al. Determination of acute vascular injury and edema in porcine carotid arteries by T2 weighted cardiovascular magnetic resonance. Int J Cardiovasc Imaging. 2012; 28(7):1717-24.
4. Pedersen SF, Thrysoe SA, Paaske WP, et al. Determination of edema in porcine coronary arteries by T2 weighted cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2011;13:52.
5. Balu N, Yarnykh VL, Chu B, et al. Carotid plaque assessment using fast 3D isotropic resolution black-blood MRI. Magn Reson Med. 2011;65:627-37.
6. Wang J, Yarnykh VL, Yuan C. Enhanced image quality in black-blood MRI using the improved Motion-Sensitized Driven-Equilibrium (iMSDE) sequence. J Magn Reson Imaging. 2010;31:1256-63.
Figures