4566
Fractional anisotropy values of pyramidal tract and motor functional recovery: intracerebral hemorrhage patients study1Neurosurgery, Sendai Medical Center, Sendai, Japan, 2Neurosurgery, Iwate Meical University, Morioka, Japan, 3Neurosurgery, Tohoku University Graduate School of Medicine, Sendai, Japan
Synopsis
Patients with ICH are sometimes treated with surgical evacuation. However, the efficacy of surgery remains unclear for recovery of motor function. We assessed the relationship between motor function outcome and sequential change of FA in patients, to explore whether motor function outcome can be predicted in the early phase. The FA values of the cerebral peduncle on day 3 could predict the motor function outcome on day 90. Patients with severe motor paresis and FA value of greater than 0.7 should be considered for surgical evacuation.
Buckground
Patients with intracerebral hemorrhage (ICH) are sometimes treated with surgical evacuation of the hematoma to save life. However, the efficacy of surgical evacuation in patients with ICH remains unclear for recovery of motor function. We assessed the relationship between improvement of motor function outcome and sequential change of fractional anisotropy (FA) values investigated in patients with ICH, to explore whether motor function outcome can be predicted in the early phase. Selection of patients for surgical hematoma evacuation was also considered.Methods
This prospective study included 23 patients with ICH. All patients underwent diffusion tensor imaging to measure the FA value five times: within 3 days, day 14, day 30, day 60, and day 90 after the onset. The regions of interest were determined on the b = 0 step of the echo planar imaging scans in the bilateral cerebral peduncles and were automatically transferred onto the FA images. The FA value was then calculated for each patient. Patients were divided into good and poor recovery groups according to the motor function outcome on day 90.Results
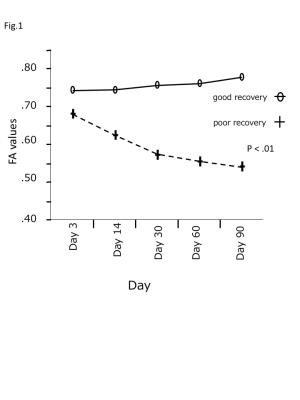
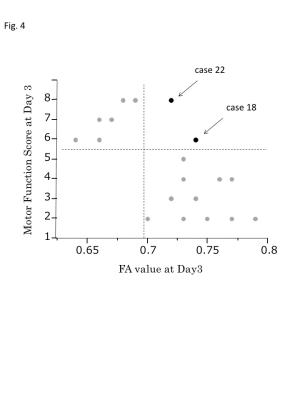
The mean FA value of the poor recovery group gradually decreased until day 90, but remained unchanged in the good recovery group (Fig. 1). The mean FA value on day 3 was significantly higher (P < .001) in the good recovery group (0.745 ± 0.0073) than in the poor recovery group (0.682 ± 0.0090) (Fig. 2). Receiver operating characteristic curve analysis showed that the FA value on day 3 could predict motor function outcome with sensitivity of 100% and specificity of 77.8% at FA value of 0.7 on day 3 (Fig. 3). The FA value and the motor function score on day 3 were independent factors for predicting the motor function outcome. Two patients with FA values of greater than 0.7 and motor function score of 6 or greater on day 3 were included in the poor recovery group (Fig. 4).Discussion
The main finding of this study was that the FA values of the cerebral peduncle on the pathological side in patients with ICH on day 3 could predict the motor function outcome on day 90. Patients with FA value of greater than 0.7 can be expected to obtain good motor function outcome. Direct injury depicted by DW imaging was previously reported to correlate with motor function outcome in patients with ICH (1). Decreased FA values in the remote pyramidal tract after stroke are associated with Wallerian degeneration. Motor neurons will be irreversibly damaged by 3 months after stroke even if not directly destroyed by hematoma in the acute stage (2-4).
The present study found that the FA values in the cerebral peduncle on day 3 already showed significant differences between the good and poor recovery groups. Conventional MR imaging can detect Wallerian degeneration by a few months after stroke onset (5-7). Reduction of anisotropy mirrors disintegration of the axonal structures, which occurs in the early phase of Wallerian degeneration, and DT imaging detects changes in water diffusion related to such beginning of pyramidal tract degeneration within the first 2 weeks after stroke, which are not yet detectable by conventional MR imaging (8). Cerebral blood flow reduction may be correlated with the FA value decrease. The cerebral flow dynamics measured by perfusion-weighted imaging demonstrated that perihematoma relative mean transit time was significantly increased and was correlated with hematoma volume (9).The present study included 2 patients with FA value of greater than 0.7 in the poor recovery group (Cases 18 and 22). In these patients, the pyramidal tract was not directly damaged by the hematoma on day 3, and the FA values of greater than 0.7 suggested good recovery. However, the FA values gradually decreased and motor function score did not recover. Although the exact reasons are difficult to explain, the pyramidal tract might have been gradually damaged after the onset. Surgical evacuation of the hematoma in the acute phase may improve motor function outcome for such patients.
Conclusion
Measurement of FA value can predict the motor function outcome. Although a large scale randomized controlled study is needed to confirm these findings, patients with severe motor paresis and FA value of greater than 0.7 should be considered for surgical evacuation. In the present study, FA values in the poor recovery group gradually decreased until day 90, suggesting that neural tracts in the poor recovery group had undergone progressive Wallerian degeneration for 90 days.
Acknowledgements
No acknowledgement found.References
(1) Karibe H, Shimizu H, Tominaga T, Koshu K, Yoshimoto T: Diffusion-weighted magnetic resonance imaging in the early evaluation of corticospinal tract injury to predict functional motor outcome in patients with deep intracerebral hemorrhage. J Neurosurg 2000;92:58-63.
(2) Yamada K, Kizu O, Ito H, Nakamura H, Yuen S, Yoshikawa K, Shiga K, Nishimura T: Wallerian degeneration of the inferior cerebellar peduncle depicted by diffusion weighted imaging. J Neurol Neurosurg Psychiatry 2003;74:977-978.
(3) Dong Q, Welsh RC, Chenevert TL, Carlos RC, Maly-Sundgren P, Gomez-Hassan DM, Mukherji SK: Clinical applications of diffusion tensor imaging. J Magn Reson Imaging 2004;19:6-18.
(4) Wieshmann UC, Clark CA, Symms MR, Franconi F, Barker GJ, Shorvon SD: Reduced anisotropy of water diffusion in structural cerebral abnormalities demonstrated with diffusion tensor imaging. Magn Reson Imaging 1999;17:1269-1274.
(5) Pujol J, Marti-Vilalta JL, Junque C, Vendrell P, Fernandez J, Capdevila A: Wallerian degeneration of the pyramidal tract in capsular infarction studied by magnetic resonance imaging. Stroke 1990;21:404-409.
(6) Inoue Y, Matsumura Y, Fukuda T, Nemoto Y, Shirahata N, Suzuki T, Shakudo M, Yawata S, Tanaka S, Takemoto K, et al.: Mr imaging of wallerian degeneration in the brainstem: Temporal relationships. AJNR Am J Neuroradiol 1990;11:897-902.
(7) Kuhn MJ, Mikulis DJ, Ayoub DM, Kosofsky BE, Davis KR, Taveras JM: Wallerian degeneration after cerebral infarction: Evaluation with sequential mr imaging. Radiology 1989;172:179-182.
(8) Thomalla G, Glauche V, Koch MA, Beaulieu C, Weiller C, Rother J: Diffusion tensor imaging detects early wallerian degeneration of the pyramidal tract after ischemic stroke. Neuroimage 2004;22:1767-1774.
(9) Butcher KS, Baird T, MacGregor L, Desmond P, Tress B, Davis S: Perihematomal edema in primary intracerebral hemorrhage is plasma derived. Stroke 2004;35:1879-1885.
Figures