4515
Automated Versus Manual Analysis of DTI and Blood Flow in Adolescents with Chronic Post-Concussive Symptoms1Radiology, Loma Linda University, Loma Linda, CA, United States, 2Pediatrics, Loma Linda University, Loma Linda, CA, United States
Synopsis
Adolescents who sustained a concussion and had persistent symptoms were scanned with DSC-PWI, to assess blood flow, and DTI. Images were compared with controls using automatically defined ROIs by registration to an atlas, and manually drawing ROIs. While both techniques showed similar trends manual ROIs has less variance within groups and therefore greater sensitivity. To detect subtle imaging changes after concussion on an individual basis, manual ROIs, despite being time intensive to define, should still be considered due to their greater sensitivity.
Purpose
Mild traumatic brain injury (TBI) including sports-related concussions (SRC) typically does not show any gross imaging findings, however approximately 14% of school age children with SRC remain symptomatic 3 months after injury (1-2). Previous studies have shown more subtle group differences with regions of white matter diffusivity changes and hypoperfusion in symptomatic patients in the chronic phase of mild TBI (3-6); however data in the pediatric population remains limited. Using both automated and manual region of interest (ROI) approaches, we investigated the anatomical distribution of white matter diffusivity changes and hypoperfusion in chronic symptomatic pediatric subjects to determine the sensitivity of each approach, with the goal of developing techniques sensitive enough to be applied to individual patients.
Methods
Twenty six adolescents (15 ± 3 years) who sustained a SRC (3–24 months before imaging) and 24 controls (12 DTI+DSC, 12 DTI only, 15 ± 3 years) were enrolled in the study. Pediatric SRC subjects were referred by a pediatric neurologist and included if they self-reported cognitive, behavioral, or emotional symptoms. Conventional 3D T1 weighted (MPRAGE, repetition time (TR) and echo time (TE) = 1950 msec and 2.26 msec, 1 mm slice thickness, field of view (FOV; 230 x 256 mm2) and DSC-PWI (SE-EPI, TR/TE = 2580/32 ms, flip angle = 90º, 5 mm slice thickness, FOV = 128 x 128, and 50 measures) were acquired using a 3.0T Siemens Tim Trio MR scanner equipped with a 12 channel receive-only head coil. For the DSC-PWI acquisition, gadolinium contrast was administered intravenously (0.1 mmol/kg). Relative CBF maps were generated using Olea Sphere (Olea Medical, Cambridge, MA, USA) using a Bayesian probabilistic estimation algorithm with automatic arterial input function selection. DTI maps (FA, AD, RD, MD) were generated using Camino. Two pediatric templates were created using ANTs (http://stnava.github.io/ANTs/), one from the 3D T1 weighted images and another from the DTI FA images. All T1 and FA images were registered to these common templates using ANTs. Additionally DSC images were registered to the subject’s T1 image using ANTs, the DSC maps DSC maps were transformed into the common T1 template space using the warp files generated by the two registrations steps above. Similarly DTI maps were transformed into the common FA template using the warp file from the FA registration. The OASIS-TRT-20 joint fusion atlas from the Mindboggle dataset7 was registered to our T1 pediatric template; standard cortical regions from the atlas were then automatically applied to all subjects DSC maps. The JHU-ICBM white matter atlas was registered to our FA pediatric template; standard DTI tracts were then automatically applied to all subjects DTI maps. Manual regions of interest, corresponding to the same cortical regions and DTI tracts that were automatically defined above, were drawn on unmodified individual DSC and DTI maps.Results
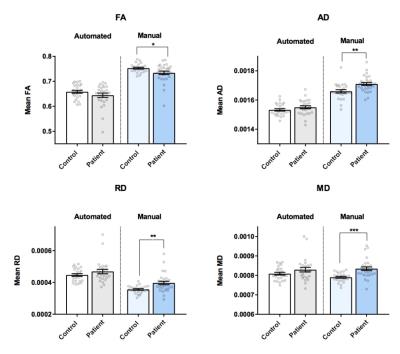
While generally of very high quality, automatically defined ROIs had some errors on the edge definition of structures, increasing variance across patients and reducing sensitivity. Manual versus automatically defined ROIs showed the same trends (Fig 1 reduced CBF and Fig 2 reduced FA) but more significant results. Automatic and manual ROIs showed hypoperfusion (reduced rCBF) in all regions, with manual ROIs showing significant changes in the occipital and temporal gray matter (Fig 1, p < 0.05) and likely reflect a diffuse reduction of metabolism or neuronal loss. Manual ROIs showed reduced FA in the genu, inferior longitudinal fasciculus (ILF), and splenium (Fig 2). Analysis of splenium showed FA changes due to both increased AD and RD.Conclusion
While the latest techniques in coregistration and automated image labeling generally show very good results, small errors at the edge of structures increase variance within groups and reduce sensitivity. Automatically defined ROIs showed the same trends as manually drawn ROIs but with less regions reaching significance. In order to maximize sensitivity manually drawing entire anatomic regions still gives the best results, and may be required to detect changes on an individual level. Significant group changes were detected in both DTI and CBF, in particular reduced FA and increased AD, RD and MD in the corpus callosum and ILF, and decreased CBF in the occipital and temporal lobes. These findings may reflect long term changes to the neurovascular unit following concussion, which likely contributes to posttraumatic headaches and long term cognitive and behavior deficits.Acknowledgements
No acknowledgement found.References
1. Ponsford J, et al. J Head Trauma Rehabil. 1999;14(4):360-375.
2. Barlow K, et al. Pediatrics. 2010;126(2):e374-381.
3. Ge Y, et al. Brain Inj. 2009;23:666-674.
4. Bonne O, et al. Psych Res. 2003;124:141-152.
5. Grossman EJ, et al. AJNR AM J Neuroradiol. 2013;34(5): 951-957.
6. Bartnik-Olson et al. J Neurotrauma. 2014; 31(17):1497-506.
7. Arno Klein, Jason Tourville. Frontiers in Brain Imaging Methods. 2012; 6:171.
Figures