4504
Evaluation of PET and MR datasets in integrated 18F-FDG PET/MRI: a comparison of different MR sequences for whole-body restaging of breast cancer patients.1Diagnostic and Interventional Radiology, University Hospital Essen, Essen, Germany
Synopsis
Simultaneous PET/MR imaging has been successfully implemented for whole-body staging of numerous tumor entities within the last four years. However, to date, the introduced study protocols were acquainted with prolonged examination times, potentially impeding patient comfort and patient compliance. The present results demonstrate the high diagnostic capability of integrated PET/MR imaging for staging patients with suspected breast cancer recurrence. Furthermore, facing the need for an optimization of dedicated MR study protocols for whole-body PET/MR imaging on oncological purposes, the present data support the application of fast, yet morphologically adequate PET/MR protocols, leaving the application of contrast-agent and DWI debatable.
Introduction
Highly accurate (re)staging of breast cancer patients is mandatory to ensure best possible individual treatment strategy, which strictly depends on the extent and distribution of the metastatic spread. Within the last years integrated PET/MR scanners have been successfully introduced into clinical imaging and the majority of initial studies could demonstrate a good staging performance for several tumor entities, including breast cancer.1,2 However, one major drawback of PET/MR imaging are prolonged examination times, potentially resulting in patient discomfort. Hence, well-defined MR protocols are needed, preserving the high diagnostic capabilities of integrated PET/MR imaging while maintaining adequate examination times.3 Therefore, the aim of the present study was to evaluate the diagnostic capability of integrated PET/MRI for staging patients with suspected breast cancer recurrence as well as to assess the diagnostic value of three MR sequences as a part of a dedicated whole-body protocol for the identification of recurrent breast cancer lesions.Methods
A total of 36 consecutive patients (mean age 58±14 years) with suspected tumor recurrence of breast cancer were prospectively enrolled for a clinically indicated whole-body PET/MR examination using a 3 Tesla Biograph mMR scanner (Siemens Healthcare, Erlangen Germany). The MR protocol comprised an T2-weighted HASTE sequence, a diffusion-weighted (DWI) EPI sequence and a post-contrast T1w VIBE sequence (sequence parameters are given in figure 1). Data analysis was performed by an experienced radiologist and a nuclear medicine physician, in consensus. First, whole-body MRI alone datasets were interpreted. Additionally, PET/MRI datasets were analyzed, while in each reading session a different constellation of available MR sequences was utilized: 1. PET/MR-HASTE/DWI, 2. PET/MR-HASTE/VIBE and 3. PET/MR-HASTE/DWI/VIBE. The readers were asked to identify the total number of tumor lesions in each imaging session. Furthermore, the diagnostic confidence for the determination of a malignant or benign lesion was qualitatively rated for each lesion in the different reading sessions, using a three-point ordinal scale (1, not confident; 2, indifferent; 3, very confident).Results
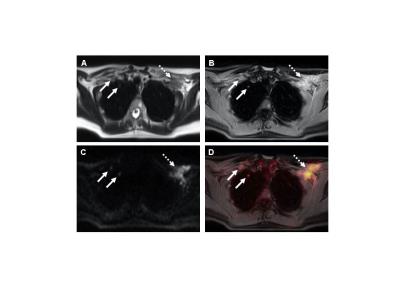
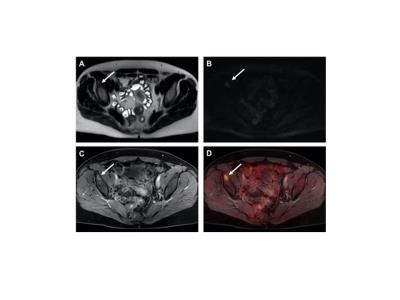
A tumor recurrence was present in 25 (69%) out of the 36 patients. On a patient-based analysis, calculated sensitivity, specificity and diagnostic accuracy of MRI alone were 88%, 91% and 89%, respectively. All three PET/MR readings showed an equivalent staging performance providing higher values for the identification of patients with a tumor recurrence (96%, 91% and 94%), while the results of MRI and PET/MRI did not reveal significant differences (p>0.05). Furthermore, 165 suspect lesions were described, comprising n=122 malignant and n=43 benign lesions. MRI alone revealed a sensitivity, specificity, and diagnostic accuracy of 81%, 85% and 82%, respectively and a confidence level (CL) of 2.24±0.71 for the identification recurrent tumor lesions. All PET/MR readings showed significantly (p<0.05) higher values than MRI alone (PET/MR-HASTE/DWI: 92%, 93%, and 92%, CL: 2.44±0.66; PET/MR-HASTE/VIBE: 93%, 93% and 93%; CL: 2.65±0.53; PET/MR-HASTE/DWI/VIBE: 94%, 95% and 94%, CL: 2.72±0.49), however, the results for the detection of tumor recurrences in the three readings using PET/MRI did not differ significantly from each other (p>0.05).Discussion
Our study illustrates the high diagnostic potential of simultaneously acquired 18F-FDG and MRI data, providing a significantly higher accuracy and diagnostic confidence for the detection of recurrent breast cancer lesions when compared to MRI alone. However, prolonged examination times of PET/MR imaging has been acknowledged as a major disadvantage of this new hybrid imaging technique causing potential patient discomfort as well as increased scan abortions. The present results demonstrate an equivalent staging accuracy of the three different reading combinations of PET/MR study protocols for the detection of breast cancer recurrences. Accordingly, the omission of DWI out of the study protocol, would enable a marked reduction of the scan duration, due to a shortening of the PET data acquisition but without sustainable effects on tumor detection. On the other hand, the exclusion of a post-contrast T1w VIBE sequences provides only limited impact on overall examination times, but might be of high benefit for patients with renal insufficiencies or known allergic reactions to contrast-media. Furthermore, considering the results of qualitative analyses, highest confidence levels for the determination of malignant and benign lesions were obtained when all three MR sequences were used for image interpretation.Conclusion
Integrated PET/MRI provides superior restaging of breast cancer patients over MRI alone. However, facing the need for an optimization of dedicated MR study protocols for fast and efficient whole-body PET/MR imaging, the application of contrast-agent and the inclusion of DWI in the study protocol seems to be debatable. Therefore, dedicated PET/MR study protocols should adapted to the individual requirements of each patient.Acknowledgements
No acknowledgement found.References
1. Sawicki LM, Grueneisen J, Schaarschmidt BM, et al. Evaluation of 18F-FDG PET/MRI, 18F-FDG PET/CT, MRI, and CT in whole-body staging of recurrent breast cancer. Eur J Radiol. 2016;85(2):459-65.
2. Melsaether AN, Raad RA, Pujara AC, et al. Comparison of Whole-Body F FDG PET/MR Imaging and Whole-Body F FDG PET/CT in Terms of Lesion Detection and Radiation Dose in Patients with Breast Cancer. Radiology. 2016:151-155.
3. Grueneisen J, Schaarschmidt BM, Heubner M, et al. Implementation of FAST-PET/MRI for whole-body staging of female patients with recurrent pelvic malignancies: A comparison to PET/CT. Eur J Radiol. 2015;84(11):2097-102.
Figures