4464
Clinical Impact of Reduced Spectral Acquisitions in Calibrated 3D Multi-Spectral Imaging Near Metal Implants1Radiology, Medical College of Wisconsin, Milwaukee, WI, United States, 2Applications and Workflow, GE Healthcare
Synopsis
We present the clinical evaluation results of a novel approach for acquisition time reduction in 3D multispectral imaging near implants. Two musculoskeletal radiologists compared standard MAVRIC SL sequences to spectrally calibrated MAVRIC SL sequences for exams of instrumented hips, knees, and shoulders. Initial results demonstrated maintenance of diagnostic information in the hips when the calibration is utilized. Rotator cuff evaluation was still limited in the shoulder using the calibrated technique but evaluation of the other structures was nearly equivalent. Calibrated imaging of the knee showed reductions of SNR, which will inform future adjustment of targeted calibrated protocols in this joint.
Clinical Question
Can calibrated 3D multispectral imaging techniques achieve the same diagnostic information as standard techniques with shorter scan times?
Impact
The amount of instrumentation placed in patients in the U.S. continues to increase. 332,000 total hip replacements and 719,000 total knee replacements were performed in 2010. This number is expected to rise due to an aging population and are being placed in younger patients1,2,3.
This results in a substantial population that will require imaging related to pain, complications, or the need to evaluate conditions occurring in close proximity to the instrumentation. Earlier placement of metallic implants also results in the higher likelihood of failure within the patient's lifetime1,2.
Osteolysis, loosening, and adverse local soft tissue reactions are well known complications that can cause devastating soft tissue injury and require complex revisions1,2,3,4,5. Early detection of complications can significantly improve morbidity and decrease the need for complex surgery.
Standard of care for orthopedic oncologic patient's is to have follow-up imaging following resection. These techniques allows standard of care practices to be utilized in the subset of patients treated with oncologic implants/instrumentation.
Approach
3D mutli-spectral imaging6,7 is the gold standard for imaging instrumentation. We employed MAVRIC SL 3D-MSI (GE)8.
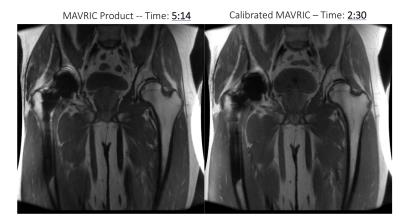
A group of consented patients underwent routine scanning with MAVRIC SL of instrumented hips, knees, and a shoulder. Additionally, 1 minute calibration scan was acquired to estimate the required number of spectral bins9. Since the length of a scan is proportionate to the number of spectral bins utilized (which is fixed in commercially available MAVRIC SL), the reduction in spectral bins, in combination with increased echo train lengths using a variable flip angle scheme10, led to decreased the scan time of an additional calibrated MAVRIC SL scan. Aside from slight variations in repetition time, all other key parameters were fixed between the two acquisitions.
Gains and Losses
Reduced acquisition times can increase patient comfort, decrease the probability of motion artifact and potentially limit the need for repeat scanning. The gain in scan time could instead be used to improve SNR or resolution, two areas where 3D-MSI is inferior to routine fast spin echo imaging1,2,3,4,5.
A smaller gain of unclear significance at this time is a reduction in ripple artifacts due to the decreased spectral bins present at areas of rapidly changing local magnetic fields11,12,13.
The potential diagnostic losses could be derived from reduce signal to noise ratios and slightly increased signal loss artifacts near implant interfaces.
Ideally, no indirect harm would come to the patient if protocols can be adjusted to reduce spectral coverage without altering diagnostic information. The challenge is to define such diagnostically neutral protocol adjustments. Here, we seek to assess a basic implementation of calibrated 3D-MSI, with nearly identical protocol settings between the compared acquisitions.
Preliminary Data
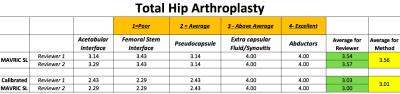
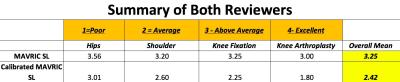
The study compared a single MAVRIC SL proton density sequence to a calibrated MAVRIC SL proton density sequence that had decreased spectral bins for exams of the hips, knees, and a shoulder.
Two musculoskeletal radiologists reviewed and graded 14 different exams. A scale of 1 to 4 was used to grade the quality of the image with respect to visualization and evaluation of the most important structures normally scrutinized clinically for each body part exam. The mean values were calculated for each structure evaluated, each body part, and across joint studies for the individual reviewers and then combined.
The results were promising for calibrated hip arthroplasty assessments. Only minor differences were observed between standard imaging and the calibrated studies. As expected there was more susceptibility artifact on the calibrated technique. However, both reviewers felt that the final diagnosis would not be significantly impacted.
Evaluation of the rotator cuff is difficult even with the use of standard MAVRIC SL imaging due to the geometry of the humeral component and inhomogeneity of the magnetic field in this region which coincides with the distal insertion of the rotator cuff3. The calibrated scan demonstrated decreased visualization of the rotator cuff. However, the structures remote from the superior aspect of the humeral component were well seen and the technique is likely still advantageous if the clinical question was not solely regarding the rotator cuff or perhaps applied to a different scan plane4,5.
With matched acquisition parameters, the calibrated approach struggled with knee exams. The cause of these shortcomings (contrast and signal quality) is likely due to SNR reductions resulting from the applied variable flip angle scheme. It is likely that calibrated 3D-MSI protocols in the knee will require reductions of parallel imaging to compensate for this reduction in SNR. Further investigations will assess such protocol adjustments.
Acknowledgements
This project was supported in part by grants from Advancing a Healthier Wisconsin Research and Education Program and GE Healthcare.
References
1). Fritz, Jan, Brett Lurie, Theodore T. Miller, and Hollis G. Potter. "MR Imaging of Hip Arthroplasty Implants." RadioGraphics 34.4 (2014): E106–E132
2). Fritz, Jan, Brett Lurie, and Hollis G. Potter. "MR Imaging of Knee Arthroplasty Implants." RadioGraphics 35.5 (2015): 1483-501.
3). Talbot, Brett S., and Eric P. Weinberg. "MR Imaging with Metal-suppression Sequences for Evaluation of Total Joint Arthroplasty." RadioGraphics 36.1 (2016): 209-25.
4).Sperling, John W., Hollis G. Potter, Edward V. Craig, Evan Flatow, and Russell F. Warren. "Magnetic Resonance Imaging of Painful Shoulder Arthroplasty." Journal of Shoulder and Elbow Surgery 11.4 (2002): 315-21.
5). Nwawka, O. Kenechi, Gabrielle P. Konin, Darryl B. Sneag, Lawrence V. Gulotta, and Hollis G. Potter. "Magnetic Resonance Imaging of Shoulder Arthroplasty." HSS Journal ® HSS Jrnl 10.3 (2014): 213-24.
6) Koch, K. M., Lorbiecki, J. E., Hinks, R. S., & King, K. F. A multispectral three-dimensional acquisition technique for imaging near metal implants. Magnetic Resonance in Medicine, (2009). 61(2), 381–390.
7) Lu, W., Pauly, K. B., Gold, G. E., Pauly, J., & Hargreaves, B. (. SEMAC: Slice encoding for metal artifact correction in MRI. Magnetic Resonance in Medicine, (2009) 62(4), 66–76.
8). Koch, K. M., A. C. Brau, W. Chen, G. E. Gold, B. A. Hargreaves, M. Koff, G. C. Mckinnon, H. G. Potter, and K. F. King. "Imaging near Metal with a MAVRIC-SEMAC Hybrid." Magnetic Resonance in Medicine 65.1 (2010): 71-82.
9) Kaushik, S. S., Marszalkowski, C., & Koch, K. M. External calibration of the spectral coverage for three-dimensional multispectral MRI. Magnetic Resonance in Medicine, (2016). 76(5), 1494–1503.
10) Busse, R., Brau, A., Vu, A., Michelich, C., Bayram, E., Kijowski, R., et al. . Effects of refocusing flip angle modulation and view ordering in 3D fast spin echo. Magnetic Resonance in Medicine, (2008), 60(4), 640–649.
11) Koch, K. M., King, K. F., Carl, M., & Hargreaves, B. A. Imaging near metal: The impact of extreme static local field gradients on frequency encoding processes. Magnetic Resonance in Medicine, (2014). 71(6), 2024–2034.
12). Dillenseger, J. P., S. Molière, P. Choquet, C. Goetz, M. Ehlinger, and G. Bierry. "An Illustrative Review to Understand and Manage Metal-induced Artifacts in Musculoskeletal MRI: A Primer and Updates." Skeletal Radiol Skeletal Radiology 45.5 (2016): 677-88.
13). Harder, J. Chiel Den, Gert H. Van Yperen, Ulrike A.
Blume, and Clemens Bos. "Ripple Artifact Reduction Using Slice Overlap in
Slice Encoding for Metal Artifact Correction." Magnetic Resonance in
Medicine 73.1 (2014): 318-24.
Figures