4455
MR arthrography of the hip using 3D isotropic SPGR reconstructed with ESPIRiT compressed sensing reconstruction and two-point Dixon fat-water separation1Department of Radiology, Stanford University School of Medicine, Stanford, CA, United States, 2GE Healthcare, 3Department of Radiology, Stanford University School of Medicine, CA, United States, 4Stanford University School of Medicine, CA, United States
Synopsis
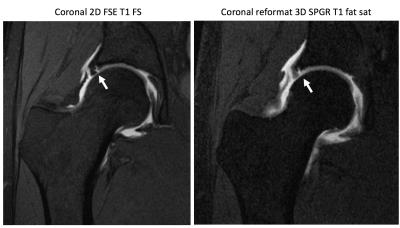
A single volumetric SPGR sequence reconstructed with ESPIRiT compressed sensing reconstruction and two-point Dixon fat-water separation was added to routine hip MR arthrogram and compared to the conventional 3-plane 2D-FSE fat-saturated T1-weighted sequences in identification of hip pathology in 25 patients. SPGR compared favorably well with T1 FS, but failed to identify 3 subtle labral tears, 1 chondral delamination and 3 low-grade ligamentum teres tears, possibly due to increased blurring associated with SPGR, decreasing overall image quality of SPGR. The relative time saving of SPGR and ability to subsequently reformat data makes this a viable technique for hip MR arthrograms.
Clinical question
Can 3D isotropic fat suppressed T1 SPGR replace conventional 3 plane 2D FSE fat saturated T1-weighted sequences in MR arthrograms of the hip for the diagnosis of labral tears, chondral pathology, and osseous abnormality?Impact
Acetabular labral tears are a common cause of hip pain, found in 22% of athletes presenting with groin pain 1 and 55% of patients with mechanical hip pain of unknown etiology 2, and are frequently associated with chondral injury 3. MR arthrography (MRA) is the imaging modality of choice for assessment of labral and chondral pathology in patients with hip pain, and aids in diagnosis of morphologic abnormalities of the proximal femur and acetabulum that occur in femoral acetabular impingement 4. Conventional protocols include 3-plane T1-weighted images with fat saturation (T1 FS) as well as a combination of proton-density and T2-weighted images, one of which is acquired in a radial imaging plane perpendicular to the femoral axis allowing comprehensive assessment of labral and chondral pathology, as well as osseous anatomy of the femoral neck. However, the radials can be challenging to set up correctly, requiring technologist training and supervision. Complete hip MRA protocols are time consuming, taking up to 45 minutes. Decreasing overall scan time by replacing conventional T1 FS sequences with a single 3D isotropic SPGR sequence would improve patient throughput, and the ability to subsequently reformat scan data at the work station may obviate the need to acquire radial images, which are often prone to prescribing errors.Approach
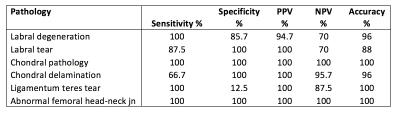
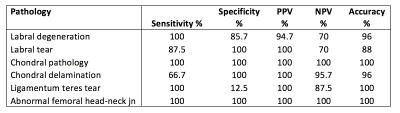
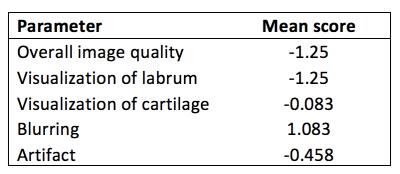
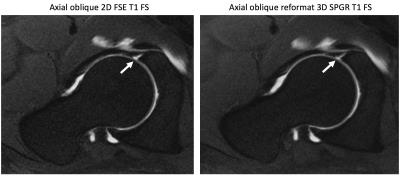
Our isotropic 3D SPGR sequence with 2 echoes is accelerated using a Poisson disk sampling pattern 5 and reconstructed using compressed sensing parallel imaging (ESPIRiT) 6 and 2-point Dixon fat-water separation. Axial SPGR (Table 1) was added to the routine hip MRA protocol and 25 patients were scanned with this new protocol with informed consent and IRB approval. SPGR images were evaluated for the presence of labral degeneration, labral tear, chondral pathology, chondral delamination, ligamentum teres tears and an abnormal femoral head-neck junction. The specificity, sensitivity, positive and negative predictive values, and accuracy for SPGR were calculated, using the T1 FS images as the “gold standard” (Table 2). Sequences were also compared and graded for overall imaging quality, visualization of labrum, visualization of articular cartilage, blurring and artifact by an experienced MSK radiologist using a 5-point scale (Table 3).Gains and losses
3D isotropic resolution sequences acquire thin continuous slices through joints, decreasing the effects of partial volume averaging, and can be used to create multiplanar reformat images from a single acquisition 7. Previous studies have shown that 3D IDEAL-SPGR has a similar sensitivity and lower specificity for detecting cartilage lesions in the hip and a higher accuracy for grading cartilage lesions compared to conventional MR arthrography sequences 8. We hope that SPGR with 0.8mm isotropic resolution will also provide equivalent diagnostic information on labral, ligamentum teres and bony pathology to the traditional 3 plane T1 FS sequences, which take approximately 9 minutes to set up and acquire in total, and may obviate the need for radial PD FS images, which take another 3 minutes to prescribe and acquire. In addition the ability to reformat the SPGR at multiple slice thicknesses and in any chosen imaging plane on the work station allows the radiologist to quickly and easily perform radial reconstructions. We anticipate that the advantages of the isotropic technique will outweigh the motion artifacts of a 3D technique.Preliminary data
SPGR had high sensitivity, specificity, and accuracy (Table 2) in the evaluation of chondral pathology and abnormalities of the femoral head neck junction. Of 21 labral tears SPGR correctly identified 18 but missed 3 tiny tears detected on T1 FS. In 3 cases of chondral delamination 1 was missed on SPGR, and of 7 ligamentum teres tears 3 low-grade partial tears were missed on SPGR. In each case the increased blurring obscured subtle abnormalities. The perceived overall image quality was lower with SPGR (Table 3), largely due to blurring and higher signal from the labrum compared to T1 FS. Susceptibility artifacts from metallic debris and small bubbles of gas were also slightly more pronounced on SPGR images, but did not obscure visualization of chondral or labral pathology.
In conclusion the 3D isotropic SPGR sequence reconstructed with ESPIRiT compressed sensing reconstruction and two-point Dixon fat-water separation provides a feasible alternative to the conventional T1 FS images and radial acquisitions in MRA of the hip, decreasing overall scan time. We anticipate that acquisition time can be further decreased with optimized sampling patterns for compressed sensing and parallel imaging.
Acknowledgements
GE Healthcare and NIH R01EB009690References
1. Narvani AA, Tsiridis E, Kendall S, et al. A preliminary report on prevalence of acetabular labrum tears in sports patients with groin pain. Knee Surg Sports Traumatol Arthrosc 2003; 11: 403–408.
2. McCarthy JC, Noble PC, Schuck MR, et al. The Otto E Aufranc Award the role of labral lesions to development of early degenerative hip disease. Clin Orthop. 2001; 393: 25–37.
3. Groh MM, Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med 2009; 2: 105–117.
4. Naraghi A, White LM. MRI of labral and chondral lesions of the hip. AJR Am J Roentgenol. 2015; 205(3): 479-490.
5. Vasanawala SS, Alley MT, Hargreaves BA, et al. Improved pediatric MR imaging with compressed sensing. Radiology 2010; 256: 607-616.
6. Uecker M, Lai P, Murphy M, et al. ESPIRiT – an eigenvalue approach to autocalibrating parallel MRI: where SENSE meets GRAPPA. Magn Reson Med 2014; 71: 990-1001.
7. Kijowski R and Gold GE. Routine 3D magnetic resonance imaging of joints. JMRI 2011; 333: 758-771.
8. Blankenbaker DG, Ullrick SR, Kijowski R, et al. MR arthrography of the hip: Comparison of IDEAL-SPGR volume sequence to standard MR sequences in the detection and grading of cartilage lesions. Radiology 2011; 261: 863-887.
Figures