4446
A clinically-validated, fast and semi-automated MR workflow for Liver Evaluation1Department of Radiology, Changhai Hospital of Shanghai, the Second Military Medical University, Shanghai, People's Republic of China, 2Application development, Siemens Shenzhen Magnetic Resonance Ltd., Shenzhen, People's Republic of China, 3MR Applications Predevelopment, Siemens Healthcare, Erlangen, Germany, 4MR Collaboration NE Asia, Siemens Healthcare, Shanghai, People's Republic of China
Synopsis
A fast and semi-automated MRI workflow for liver examinations with approximately 12mins of total examination time was proposed and evaluated with liver patients using CT or histo-pathology as reference. 28 patients suspected of liver disease were enrolled in this study. The results show a good concordance between findings on MRI and the chosen reference standard. This indicates that the proposed fast MRI workflow has the capability to be used for diagnostic purposes in clinical routine while being highly time efficient at the same time.
Clinical Question
Is it possible to achieve CT-like fast & semi-automated MR contrast-enhanced liver exams without compromising diagnostic value?Impact
MR imaging of the liver is one of the most time-consuming MR examinations, with typical exam times of about 30minutes and more, and a lack of standardization. Patients typically undergoing liver MRI often are severely ill, have comorbidities and problems to lie still for long time. CT has the advantage of being much faster and normally takes ~10mins on-bed time for a liver examination. However, CT exposes the patient to radiation with associated risks and has been shown to be inferior to MRI in terms of characterizing soft tissues.Approach
We propose a fast and semi-automated MR program for liver examination, with ~12mins total exam time (comparable with CT scan time), using automatic FOV adjustments and auto-bolus detection functionalities provided by the Abdomen Dot engine.
The proposed MRI program was implemented on a 3T scanner (MAGNETOM Skyra, Siemens, Erlangen, Germany) and included the following protocols:
1. Localizer with 3 standard orientations in one breath-hold of 18s. The localizer data were used by the Auto Positioning functionality of the following sequences.
2. Coronal T2 HASTE in one breath-hold of 20s, FOV=425x340mm2, scan matrix=256x240, TE =97ms, TR=1000ms, slice thickness=6mm, slice number=20.
3. Axial T2 BLADE with respiratory triggering, with Echo train length=42, FOV=400x400mm2, scan matrix =320x320, TE=79ms, slice thickness=6mm, slice number=28, iPAT factor =2; Scan duration varied from 2 to 4 mins.
4. T1 VIBE with 2 echoes and DIXON reconstruction in one breath-hold of 15s, acting as a) pre-contrast in-and-opposed-phase T1 weighted and b) as pre-contrast T1 weighted scan. FOV =325x400mm2, scan matrix=195x320, iPAT factor=3, TE=1.26/2.43ms, TR=3.97ms, flip angle =120.
5. EPI DWI sequence (with slice selective shimming (iShim), prototype) in two breath-holds of 36s, with a single high b value of 1000s/mm2, FOV=400x400mm2, scan matrix =256x256 with interpolation, TE=61ms, TR=3100ms, slice thickness =6mm, slice number =30, iPAT factor=2.
6. Auto bolus detection with 2D FLASH sequence, having temporary resolution of ~0.8s with automatic ROI placement based on automatic segmentation of the aorta on the localizer data. After starting this sequence, the contrast agent was injected and the arrival of the bolus was detected automatically.
7. Post-contrast T1 VIBE for arterial, venous and delayed phase measurement. Imaging parameters are identical with those of pre-contrast T1 VIBE (s. step4), except for fat saturation, instead of DIXON.
Slice auto-alignment and Auto-FOV was switched on for all above sequences. Automatic voice commands were applied in all breath-hold sequences.
The sum of pure measurement time of all sequences in the program ranged from 5.7mins to 7mins.
Gain and Losses
Our fast MRI workflow for liver evaluation achieves a short and reproducible measurement time that is comparable with CT exams. Additionally, the functionalities of slice auto-alignment, auto-FOV, auto-voice command and auto-bolus detection release technicians’ workload and increase the consistency of image qualities among patients and technicians.Preliminary data
28 patients (mean age 54.1 year; range 35-66 years) suspected of liver disease, who were scheduled for a CT liver exam or liver biopsy were enrolled in this study. To evaluate the actual measurement duration of the proposed program, the technicians were required to measure the scan duration of 10 patients, avoiding any non-work related interruption. The duration of the whole program was calculated as: Measurement duration = The Ending time of the last sequence - The start time of the first sequence. The diagnostic results based on MR data were compared with findings of liver CTs or liver biopsy.
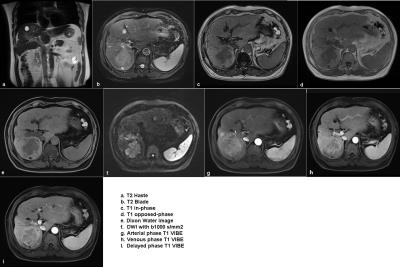
The scan time estimated in a subcohort of 10 patients was 12min01s ± 34s (mean ± std). All 28 patients had liver CT scans or liver biopsy. While 25 patients had CT scans, 4 patients had liver biopsy, and 1 patient had both CT liver scan and biopsy. Among these patients, MR findings in 23/25 cases were concordant with CT results and 3 of 4 cases were confirmed with biopsy. Figure 1 shows example images of the performed liver MRI examination.
The results of this study show that the proposed fast MRI workflow provides similar diagnostic information as the chosen reference standard while being highly time-efficient. These results should be confirmed in a future study with a larger patient population and more biopsy cases.
To conclude, the proposed fast and automatic MRI workflow allows to achieve image quality fully sufficient for diagnostic purposes while preserving a short and reproducible time slot similar to a CT liver scan by applying intelligent assistant methods to streamline the workflow.