4412
Magnetic Resonance Imaging of Collateral Networks in Moyamoya Angiopathy at 7 Tesla1Erwin L. Hahn Institute for MRI, University of Duisburg-Essen, Essen, Germany, 2Department of Neurosurgery, University Hospital Essen, University of Duisburg-Essen, Essen, Germany, 3Department of Neurosurgery, Graduate School of Biomedical and Health Sciences, Hiroshima University, Japan, 4Department of Neurology, Alfried Krupp Hospital, Essen, Germany, 5Institute of Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Giessen, Giessen University, Giessen, Germany, 6High Field and Hybrid MR Imaging, University Hospital Essen, University of Duisburg-Essen, Essen, Germany, 7Medical Physics in Radiology, German Cancer Research Center (DKFZ), Heidelberg, Germany
Synopsis
Collateral networks in Moyamoya angiopathy (MMA) have a complex angioarchitecture. Delineation of deeply seated collateral networks (DSCNs) and image quality were prospectively evaluated in 10 patients using 7 Tesla TOF MRA and MPRAGE in comparison with conventional DSA. Seventy DSCNs were detected in DSA, 79 in TOF MRA, and 54 in MPRAGE. Detection of DSCNs was significantly better in TOF MRA than in DSA and MPRAGE. TOF MRA and DSA image quality were comparable, both were better than MPRAGE. Delineation of DSCN pathways in MMA using 7 Tesla TOF MRA was excellent and comparable to DSA.
Introduction
Collateral networks in Moyamoya angiopathy (MMA) have a complex angioarchitecture difficult to comprehend in conventional examinations. This prospective study aimed to evaluate morphologic patterns and the delineation of deeply seated collateral networks (DSCNs) using ultra-high-field magnetic resonance angiography (MRA) in comparison with the current gold standard conventional digital subtraction angiography (DSA).Materials and Methods
Ten adult patients suffering from MMA underwent 7 Tesla (T) TOF MRA and MPRAGE, additionally to the standard clinical workup with conventional DSA. The study group was comprised of 3 male and 7 female patients. The mean age was 34 years (range: 21 – 58 years). The study was conducted according to the principles expressed in the Declaration of Helsinki and was approved by the local university institutional review board. Written informed consent was obtained before each examination. Ultra-high-field 7 T images were acquired on a whole-body MRI system (Magnetom 7 T, Siemens Healthcare GmbH, Erlangen, Germany) utilizing a 1/32-channel transmit/receive head coil (Nova Medical, Wilmington, USA). High-resolution MRA was acquired with a customized 3D fast low angle shot (FLASH) TOF pulse sequence1, 2 (voxel size of 0.22 × 0.22 × 0.41 mm3) and with a modified MPRAGE sequence3, 4 (voxel size 0.7 × 0.7 × 0.7 mm3). Six-vessel DSA was performed using a Siemens Axiom Artis angiography suite (Siemens Healthcare GmbH, Erlangen, Germany). Images were analyzed by four experienced raters in consensus reading. DSCNs were classified according to location and connecting vessels. Overall image quality and presence of artifacts were rated on a five-point scale (5 = excellent, 4 = good, 3 = moderate, 2 = poor, and 1 = non-diagnostic). Collateral networks were rated utilizing a five-point scale (5 = excellent, collateral networks were obviously detected with clear identification of the vessel course and high vessel-tissue contrast; 4 = good, collateral networks were well detected with lower vessel-tissue contrast; 3 = moderate, collateral networks were partially invisible but still adequate for diagnosis; 2 = poor, collateral connections were scarcely demonstrated but sufficient to presume their existence; and 1 = no collateral networks detected). Delineation of collateral networks was analyzed by the McNemar test. Image quality was compared using Wilcoxon signed-rank tests.Results
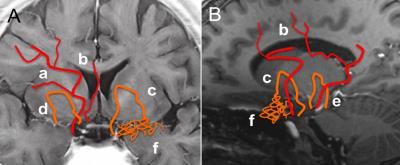
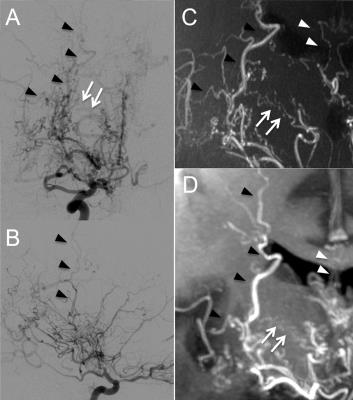
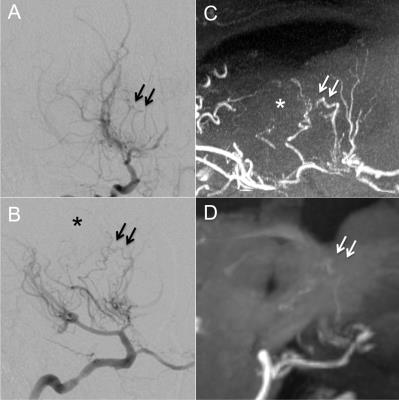
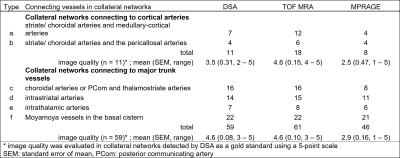
All examinations were successfully performed without occurrence of adverse events. DSCNs were classified into 2 major categories (connection to cortical vessels and connection to major trunk vessels) with a total of 6 pathways (Figure 1 a – f). Eleven collateral networks connecting to cortical arteries were detected in DSA, 18 in TOF MRA and 8 in MPRAGE. Whereas 59 collateral networks connecting among major trunk vessels were detected in DSA, 61 in TOF MRA and 46 in MPRAGE. All collateral networks detected in DSA were excellently delineated in TOF MRA and 54 of 70 (77.1%) in MPRAGE. Nine anastomoses were identified by MRA (TOF: n = 9, MPRAGE: n = 3) not visible in DSA images. Detection of DSCNs was significantly better in TOF MRA than in either DSA or MPRAGE (p < 0.01). The mean overall image quality was 4.83 in DSA, 4.92 in TOF MRA and 4.75 in MPRAGE. Overall image quality showed comparable results for DSA and TOF MRA (p = 1.0); however, both were better than MPRAGE (p < 0.0001). In collateral pathways to cortical arteries, the image quality of TOF MRA proved to be significantly better than DSA (p = 0.0468) or MPRAGE (p = 0.0234); however, the image quality between MPRAGE and DSA was comparable (p = 0.5508). For anastomoses to major trunk vessels, image quality of 7 Tesla TOF MRA and DSA were comparable (p = 1.0); however, both were better than MPRAGE (p < 0.0001). The morphologic characteristics and detected number of DSCNs as well as image quality of each imaging techniques are summarized in Table 1. Imaging results of a patient with anastomoses to cortical vessels are shown in Figure 2, images of a patient with anastomoses to major trunk vessels are presented in Figure 3.Discussion and Conclusion
In the presented study, 7 T MRA could delineate DSCNs in MMA in a clinical setting. With respect to submillimeter collateral vessels visualization by 7 Tesla TOF MRA was comparable with DSA. The applied 7 T MPRAGE sequence could visualize some collateral networks, but was inferior to 7 T TOF and DSA. For further morphological and pathophysiological research on submillimeter collateral networks in MMA, 7 Tesla TOF MRA is a very promising imaging modality.Acknowledgements
The research leading to these results has received funding from the Interne Forschungsförderung Essen (IFORES), University Hospital Essen, University Duisburg-Essen.References
1. Wrede KH, Johst S, Dammann P, et al. Improved cerebral time-of-flight magnetic resonance angiography at 7 Tesla-feasibility study and preliminary results using optimized venous saturation pulses. PLoS One 2014:9:e106697.
2. Johst S, Wrede KH, Ladd ME, et al. Time-of-flight magnetic resonance angiography at 7 T using venous saturation pulses with reduced flip angles. Invest Radiol 2012:47:445-50.
3. Wrede KH, Johst S, Dammann P, et al. Caudal image contrast inversion in mprage at 7 Tesla: Problem and solution. Acad Radiol 2012:19:172-8.
4. Umutlu L, Theysohn N, Maderwald S, et al. 7 Tesla MPRAGE imaging of the intracranial arterial vasculature: Nonenhanced versus contrast-enhanced. Acad Radiol 2013:20:628-34.
Figures