4397
MR imaging in the prediction of aggressive histological features in papillary thyroid carcinoma1Radiology, Central Hospital of Minhang District, Fudan University, Shanghai, People's Republic of China
Synopsis
Purpose To investigate the value of magnetic resonance imaging (MRI) features for prediction of tumor aggressiveness in papillary thyroid cancer (PTC). Method A consecutive series of 119 lesions with PTC were preoperatively evaluated by MR imaging. A multivariate analysis was performed to predict tumor aggressiveness by 18 independent variables. Results Multivariate analysis demonstrated that lesion size classification and tumor margin on delayed contrast-enhanced images were the independent predictors of high aggressive PTC. Conclusion Lesion size classification and tumor margin on delayed contrast-enhanced images can be used preoperatively to estimate the risk of high aggressive of PTC.
Introduction/Purpose
Initial therapeutic decision-making of papillary thyroid carcinoma (PTC) depends on pre-operative risk stratification designed to evaluate the presence of PTC with aggressive features. While fine-needle aspiration (FNA) is the one of the most accurate and cost-effective method for evaluating thyroid nodules, but this provides only minimal information with regard to tumor aggressiveness (1). Routine neck ultrasonography cannot reliably exclude minor extrathyroidal extension (ETE) (2). The purpose of this study was to identify the magnetic resonance imaging (MRI) features that can be used to predict tumor aggressiveness in patients with PTC.Method
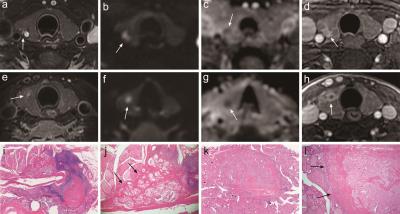
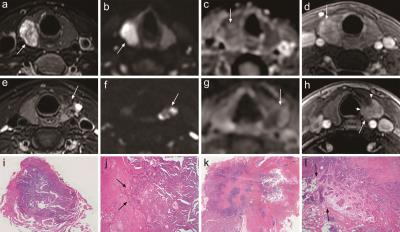
This retrospective study, 119 lesions with PTC underwent MRI with T1-weighted, T2-weighted, diffusion-weighted magnetic resonance imaging (DWI-MRI) and contrast material–enhanced sequences prior to thyroidectomy. MRI examination was performed with a GE EXCITE HD 1.5 T MR scanner (GE healthcare, USA) using 8-channel special neck coil (Chenguang Medical Technology Ltd, Shanghai, China). DWI was performed using single-shot spin echo, echo planar imaging (EPI) sequence with the following diffusion gradient b factors: 800 s / mm2. In the contrast-enhanced protocol, respiratory gating was performed during each scanning phase. The inclusion criteria were: lesions in patients who underwent enhanced MRI within 1 month before surgery. The exclusion criteria were: (1) lesion size less than 7mm (identified during histopathologic examination and reported), because it is difficult for MRI to detect; (2) lesions with poor image quality deemed to be non-diagnostic after a review of the images; (3) smaller lesions in patients who have multifocal PTCs, because its aggressiveness maybe was overestimated. Finally, 62 lesions were included for further analysis. Tumor aggressiveness was defined by surgical histopathology. Tumor size, apparent diffusion coefficients (ADC) value and MRI features on images were obtained for each patient. Descriptive statistics for tumor aggressiveness PTCs, and the sensitivity, specificity and accuracy of individual features were determined. A multivariate logistic regression model was developed to identify features that were independently predictive for tumor aggressiveness. Analyses of receiver-operating characteristic (ROC) curve were performed.Result
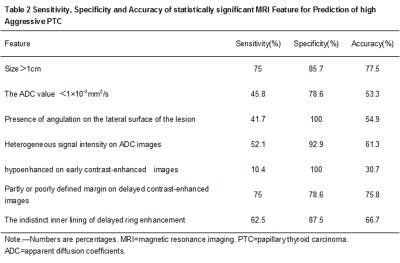
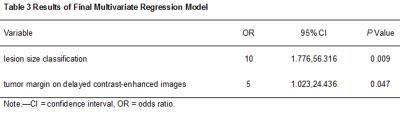
High aggressive PTC differed from low aggressive PTC in size (P=0.016), size classification (P=0.000), ADC value (P=0.01), ADC value classification (P=0.029), angulation on the lateral surface of the lesion (P=0.009), signal intensity heterogeneity on ADC images (P=0.003), early enhancement degree (P=0.000), tumor margin on delayed contrast-enhanced images (P=0.000), inner lining of delayed ring enhancement (P=0.028). The logistic regression model showed lesion size classification and tumor margin on delayed contrast-enhanced images as strongest independent predictors of high aggressive PTC (odds ratio:10; 95% confidence interval:1.776, 56.316; P=0.009 and odds ratio:5; 95% confidence interval:1.023, 24.436; P=0.047), with an accuracy of 83.9%. The area under ROC curve for ADC value and lesion size were 0.682 and 0.81, respectively.Discussion
For PTC patients, grading of tumor aggressiveness is the most critical information needed for treatment planning, as it is heavily tied to the extent of surgery (lobectomy vs near total or total thyroidectomy) and whether PCND for removal of lymph nodes is needed. The risks of near total or total thyroidectomy are significantly greater than that of thyroid lobectomy (3). The most salient argument against routine application of PCND is that it may increase the risk of complications of thyroidectomy, such as recurrent laryngeal nerve injury and hypoparathyroidism, especially if the surgeon is relatively inexperienced in the procedure (4). Thyroid lobectomy without PCND may be sufficient as initial treatment for low aggressive PTC. The results of our study demonstrated that a prediction model derived from lesion size classification and tumor margin on contrast-enhanced images demonstrated as a useful tool for estimating the probability of high or low aggressive PTC, which allowed the clinician to identify patients that are likely to benefit from more aggressive initial therapy.Conclusion
ADC value, angulation on the lateral surface of lesion, heterogeneous signal intensity on ADC images, enhancement degree on early contrast-enhanced images and the inner lining of delayed ring enhancement helped in differentiating high and low aggressive PTCs. Lesion size classification and tumor margin on contrast-enhanced images are features that may also help in differentiating high and low aggressive PTCs. MRI features may provide a useful tool for determining PTC aggressiveness in patients.Acknowledgements
We thank the financial support from the Minhang district of Shanghai Science and Technology Committee (grant 2015MHZ026, 2013MHZ016).References
1.Baloch ZW, LiVolsi VA, Asa SL, Rosai J, Merino MJ, Randolph G, Vielh P, DeMay RM, Sidawy MK, Frable WJ 2008 Diagnostic terminology and morphologic criteria for cytologic diagnosis of thyroid lesions: a synopsis of the National Cancer Institute Thyroid Fine-Needle Aspiration State of the Science Conference. Diagnostic cytopathology 36:425-437.
2.Lee CY, Kim SJ, Ko KR, Chung KW, Lee JH 2014 Predictive factors for extrathyroidal extension of papillary thyroid carcinoma based on preoperative sonography. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine 33:231-238.
3.Kandil E, Krishnan B, Noureldine SI, Yao L, Tufano RP 2013 Hemithyroidectomy: a meta-analysis of postoperative need for hormone replacement and complications. ORL; journal for oto-rhino-laryngology and its related specialties 75:6-17.
4.Carling T, Carty SE, Ciarleglio MM, Cooper DS, Doherty GM, Kim LT, Kloos RT, Mazzaferri EL, Sr., Peduzzi PN, Roman SA, Sippel RS, Sosa JA, Stack BC, Jr., Steward DL, Tufano RP, Tuttle RM, Udelsman R, American Thyroid Association Surgical Affairs C 2012 American Thyroid Association design and feasibility of a prospective randomized controlled trial of prophylactic central lymph node dissection for papillary thyroid carcinoma. Thyroid : official journal of the American Thyroid Association 22:237-244.
Figures