4389
Discriminatory ability of MRSI and DW-MRI in prostatic diseases in biopsy naïve men with PSA 4-10 ng/ml1Department of NMR and MRI Facility, All India Institute of Medical Sciences, New Delhi, Delhi, India, 2Department of Radiodiagnosis, King George's Medical University, Lucknow, India, 3Department of Urology, All India Institute of Medical Sciences, New Delhi, Delhi, India, 4Division of Biostatistics and Epidemiology, Department of Biomedical Sciences, Texas Tech University Health Sciences Center, El Paso, Texas, TX, United States, 5Department of Radiodiagnosis, All India Institute of Medical Sciences, New Delhi, New Delhi, India, 6Department of Pathology, All India Institute of Medical Sciences, New Delhi, New Delhi, India
Synopsis
Multivariate approach of including different MR parameters offer a holistic view of entire data, which could provide better approach in differentiating various prostatic diseases. This approach may help in reducing the burden of unnecessary biopsy in men with PSA 4-10 ng/ml. we evaluated discriminatory ability of MRSI and DW-MRI in prostatic diseases in biopsy naïve men with PSA 4-10 ng/ml. The combined model (PSA + ADC + metabolite ratio) showed highest discriminatory ability in various prostatic diseases with AUC of 89% in men with clinically challenging group of PSA.
Abstract
Introduction: Prostate specific antigen (PSA), digital rectal examination (DRE), and transrectal ultrasound (TRUS) are the mainstay to diagnose prostate abnormalities. These methods have some limitations in detecting prostate cancer (PCa). Pre-biopsy multiparametric MRI (mpMRI) is an emerging imaging method in the early detection of prostate cancer.1 Multivariate approach of including different MR parameters offer a holistic view of entire data, which could provide better approach in differentiating various prostatic diseases and therefore could reduce burden of unnecessary biopsy in men with PSA 4-10 ng/ml. Thus, the aim of the study was to evaluate individual and combined performance of pre-biopsy MRSI and DW-MRI in men with PSA 4-10 ng/ml in differentiating benign with PCa.
Methods: A total of 137 men with gray zone of PSA underwent pre-biopsy mpMRI at 1.5T MR scanner (AVANTO, Siemens Health Care, Germany) using endorectal coil coil (Medrad Inc., Pittsburgh, PA) in combination with pelvic phased array coil. After conventional T1W and T2W, MRSI data were subsequently acquired with the following parameters: TR = 1300 ms, TE = 120 ms, voxel size = 5 × 5 × 5 mm3, FOV = 220 mm, number of signal averages = 3. DW-MRI was performed in the transverse plane using single shot diffusion-weighted echo planar imaging (DWI-EPI) pulse sequence. Slice position in DW-MRI was matched to the transverse T2W images. The following parameters were used for DW-MRI: TR = 3000 ms, TE = 96 ms, slice thickness = 5 mm without interslice gap, and bandwidth = 1500 Hz. Five different b ‐values (0, 250, 500, 750 and 1000 s/mm2) were used to acquire different DW images. Unadjusted and adjusted logistic regression analysis were carried out for obtaining association of cofactors with pathological outcome. Stepwise multivariable logistic regression was used with 10% entry and 5% exclusion level of significance. Receiver operating characteristics (ROC) analysis was carried out to assess the diagnostic performance and findings were summarized using area under the curve (AUC) (SPSS 21.0, IBM Corp., Armonk, NY, USA; STATA 12.1, STATA Corp., College Station, Texas, USA).
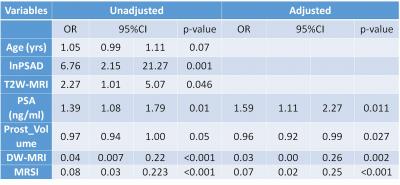
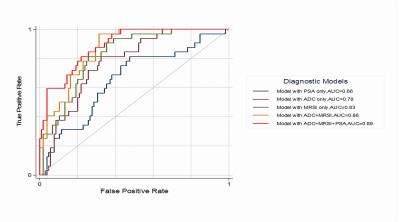
Results: Diagnostic accuracy was calculated for various MR methods at the predetermined cut-offs (metabolite ratio <1.2 and ADC values <1.17 x 10–3 mm2/s) for our study population (Table 1). Multivariable analysis showed four significant important predictors (ADC, metabolite ratio, PSA, and prostate volume) for the diagnosis of PCa (Table 2). Further, PSA had the least AUC in differentiation of benign with PCa (Figure 1). ADC (AUC = 78%) values showed moderate performance as compared with metabolite ratio (AUC = 83%). The combined model (PSA + ADC + metabolite ratio) showed highest discriminatory ability in various prostatic diseases with AUC of 89% (Figure 1).
Discussion: Differentiation of benign with malignant prostatic disease is increasingly important in men with clinically challenging group of PSA (4-10 ng/ml). Most previous studies have used post-biopsy mpMRI studies to differentiate benign with the PCa.2, 3 Pre-biopsy MR helps to avoid post-biopsy haemorrhage artefacts and it prevents delay between MR examination and biopsy. Perdona et al. evaluated the combined potential of MRSI and DCE-MRI in men with PSA < 10 ng/ml that showed the diagnostic accuracy, sensitivity, specificity, NPV and PPV of 85%, 71%, 48%, 91%, 19%, respectively.4 Our results show a marked improvement in the discriminatory ability of combined MR methods with the PSA in pre-biopsy set up. We achieved 89% AUC after combining all MR methods with the PSA in our study population. Therefore, a significant number of unnecessary biopsies could be avoided using pre-biopsy mpMRI methods in men with PSA 4-10 ng/ml.
Conclusion: The combined pre-biopsy MRSI and DW-MRI with PSA will provide a greater discriminatory ability of various prostatic diseases in men with clinically challenging group of PSA, non-invasively.
Acknowledgements
No acknowledgement found.References
1. Turkbey B, Brown AM, Sankineni S, et al. Multiparametric prostate magnetic resonance imaging in the evaluation of prostate cancer. CA Cancer J Clin 2016; 66: 326-36.
2. Zakian KL, Sircar K, Hricak H, et al. Correlation of proton MR spectroscopic imaging with gleason score based on step-section pathologic analysis after radical prostatectomy. Radiology 2005; 234: 804-14.
3. Kobus T, van der Laak JA, Maas MC, et al. Contribution of Histopathologic Tissue Composition to Quantitative MR Spectroscopy and Diffusion-weighted Imaging of the Prostate. Radiology. 2016;278:801-11.
4. Perdona S, Di Lorenzo G, Autorino R, et al. Combined magnetic resonance spectroscopy and dynamic contrast-enhanced imaging for prostate cancer detection. Urol Oncol 2013; 31: 761-5.
Figures