4364
Evaluation of tumor oxygenation following radiation and PS-targeting antibody therapy in an orthotopic lung cancer model1Radiology, Univ Texas Southwestern Medical Center, Dallas, TX, United States, 2Hamon Center for Therapeutic Oncology Research, Univ Texas Southwestern Medical Center, Dallas, TX, United States, 3Radiation Oncology, Univ Texas Southwestern Medical Center, Dallas, TX, United States, 4Surgery, Univ Texas Southwestern Medical Center, Dallas, TX, United States
Synopsis
Combining phosphatidylserine (PS)-targeting monoclonal antibodies with radiation therapy can potentially enhance treatment efficacy. Oxygenation is important in radiation therapy response and could influence future treatment design. Oxygen enhanced MRI was used to examine changes in oxygenation in orthotopic lung tumors in rats treated by radiation or radiation plus a PS-targeting antibody. Orthotopic tumors were well oxygenated and responsive to oxygen breathing challenges before and after treatment. Combination therapy appeared to be more effective in tumor control than radiation alone.
Purpose
Radiation therapy is a common treatment for lung cancer. Bavituximab, a phosphatidylserine (PS)-targeting, chimeric monoclonal antibody, stimulates innate and adaptive anti-tumor immune responses and is currently in clinical trials for several cancers [1] including non-small cell lung cancer. Previous studies had shown that exposure of PS is enhanced by radiation [2]. Therefore, combining a PS-targeting agent with radiation therapy could enhance treatment efficacy. Oxygenation is an important parameter in the effectiveness of radiation therapy [3]. To guide the design of combination treatment in the future, we performed blood oxygen level dependent (BOLD) and tissue oxygen level dependent (TOLD) MRI to observe the changes in tumor oxygenation following radiation or radiation combined with a PS targeting antibody using an orthotopic lung cancer model in nude rats.Methods
A549-luc human lung cancer cells were surgically implanted in the right lung of thirteen nude rats. Tumor growth was monitored by bioluminescent imaging. The animals were divided into three groups. Control Group (n = 4) received no treatment. IR Group (n = 4) received three fractions of irradiation in one week (12 Gy/fraction). Combination Group (n = 5) received three fractions of irradiation in one week (12 Gy/fraction) in combination with 2aG4 (a murine version of bavituximab; 4 mg/kg, twice/week for two weeks, concurrent with IR for the first three doses). Baseline and post-treatment MRI were acquired about 2.5 weeks apart using a horizontal bore 4.7-T magnet with a rat body coil. Animals were sedated with isoflurane and kept warm using a circulating warm water blanket. Animal body temperature, respiration and heart rates were monitored and respiration and ECG signal were used as an external trigger with a small animal physiological monitoring system throughout the experiment [4]. Interleaved BOLD (multi-echo gradient echo; TR = 150 ms, ten echo time from 2 to 29 ms, flip angle = 20°) and TOLD (gradient echo; TR/TE = 20/2ms, flip angle = 45°) MRI were acquired with the intervention of an oxygen breathing challenge (from air to 100% O2). BOLD was acquired with ECG triggering and TOLD was acquired with free breathing. Images were acquired in sagittal plane. Data were analyzed using home-written Matlab scripts to derive %ΔSI BOLD, %ΔSI TOLD and T2* values.Results
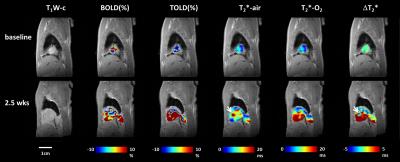
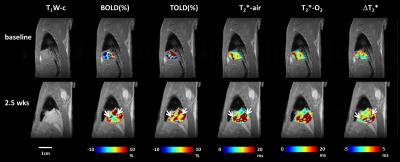
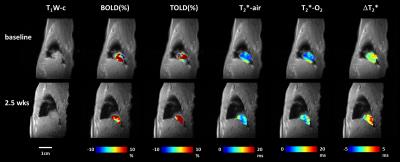
Irradiation alone did not show obvious therapeutic efficacy compared with the Control Group, while all tumors receiving the combination therapy showed stable or decreased tumor size, as observed with MRI. Most of the tumors showed a positive response to oxygen challenge at baseline in %ΔSI BOLD, %ΔSI TOLD and T2* values. Distinct heterogeneity was observed within each tumor and between tumors. Reference muscle on the other hand showed much smaller variation within the ROI and between animals. Increased response to oxygen breathing was observed in the control tumor 2.5 weeks after baseline (Fig. 1). Similarly, tumors receiving radiation treatment which continued to grow, exhibited increased response to oxygen (Fig. 2). Some areas in the tumors exhibited very high T2* values during air breathing and were less responsive to oxygen challenge (arrows in Figs. 1 & 2) potentially consistent with necrosis. Figure 3 shows a representative tumor receiving combination therapy, which exhibited a reduction in volume. Slightly higher response to oxygen challenge was observed and no obvious necrotic region was found in the tumor.Discussion
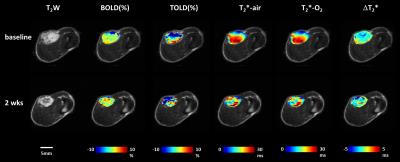
The orthotopic A549 lung tumors were less responsive to radiation than previously reported in subcutaneous A549 tumors at the same dose. Subcutaneous tumors were however less responsive to oxygen breathing challenge (Fig. 4). This preliminary observation echoed reports for mouse lung tumor models [5]. As the tumor volume increased, subcutaneous tumors tend to become less responsive to oxygen challenge suggesting incipient hypoxia. Meanwhile the orthotopic lung tumors remained highly responsive to oxygen breathing as they grew, likely due to the extensive blood supply in the lung tissue.Conclusion
Combination therapy of irradiation and PS-targeting antibody showed excellent tumor control, while irradiation alone was not effective. Multiparametric MRI showed orthotopic lung tumors were well-oxygenated and highly responsive to oxygen breathing challenge even at large size, which was distinct from subcutaneous tumor models.Acknowledgements
Supported in part by funds from CPRIT MIRA RP120670-P3; NIH 1P30 CA142543, EB015908, S10 RR028011.References
1. Gerber, D.E., et al., Clin. Cancer. Res., 17, 6888-96 (2011).
2. Zhou, H., et al., J. Biomed. Nanotechnol., 10, 846-855 (2014).
3. Tatum, J.L., et al., Int. J. Radiat. Biol., 82, 699-757 (2006).
4. Kubo, S., et al., Magn. Reson. Med., 56, 698-703 (2006).
5. Graves, E.E., et al., Clin. Cancer. Res., 16, 4843-52 (2010).
Figures