4359
Evaluation of HCC Response to Loco-regional Therapy: Validation of Response Criteria with MRI using Explant as a Reference1Translational and Molecular Imaging Institute, New York, NY, United States, 2Institute of Diagnostic and Interventional Radiology, University Hospital Zurich, Zurich, Switzerland, 3Department of Radiology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 4Department of Pathology, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Synopsis
We assessed the performance of various imaging response criteria for the prediction of complete pathologic necrosis (CPN) of hepatocellular carcinoma post locoregional therapy on liver explant. Patients who underwent liver transplantation after locoregional therapy were included in this retrospective study. All patients underwent MRI using routine liver protocol within 90 days of liver transplant. RECIST, mRECIST, EASL, percentage of necrosis on subtraction images, and DWI (signal intensity and ADC) were assessed. CPN was retrospectively assessed in all tumors at histopathology. mRECIST, EASL, percentage of necrosis and signal intensity on DWI were all significant predictors of CPN while RECIST and ADC criteria were not.
Purpose: To assess the performance of various imaging response criteria for the prediction of complete pathologic necrosis (CPN) of hepatocellular carcinoma (HCC) post locoregional therapy using liver explant as the reference.
Methods: This IRB approved retrospective study included 61 patients (M/F 46/15, mean age 60y) who underwent liver transplantation after locoregional therapy with transarterial chemoembolization plus radiofrequency or microwave ablation (n=56) or 90Yttrium radioembolization (RE, n=5). Imaging was performed within 90 days of liver transplantation using 1.5T or 3T systems using a routine liver MRI protocol including T2 HASTE, axial fat suppressed FSE T2WI, T1WI in- and out-of-phase, DWI [using 3 (50, 400, and 800) or 4 b values (0, 50, 500, and 1000 s/mm2)] and contrast-enhanced T1WI (CE-T1WI) with subtraction. The following criteria were assessed by 3 independent readers: RECIST1, modified RECIST (mRECIST)2, European Association for the Study of the Liver (EASL)3 criteria, percentage of necrosis on subtraction images (on arterial and portal venous phases), and DWI: qualitative (isointense vs. high signal intensity on high b value) and quantitative (ADC). Degree of tumor necrosis was retrospectively assessed in all index tumors at histopathology. Intraclass correlation coefficient (ICC) and Cohen’s kappa were used to assess inter-reader agreement. Logistic regression and ROC analyses were used to determine predictors of CPN.
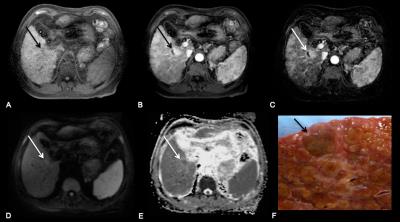
Results: 97 HCCs (mean size 2.3±1.3 cm) including 28 with CPN were evaluated. There was excellent inter-reader agreement with ICC of 0.77-0.86 for all methods, thus combined data from all readers is shown. mRECIST, EASL, % of necrosis (arterial and portal venous phases) and signal intensity were all significant (p < 0.001) predictors of CPN while RECIST and ADC were not (Figure 1 and 2). mRECIST, EASL and percentage of necrosis performed similarly with AUCs of 0.810-0.815 (sensitivity 86.9% and specificity of 73.9%-74.4%) while the performance of high signal intensity on DWI was lower with AUC of 0.622 (sensitivity 81% and specificity of 43.3%).
Discussion: mRECIST, EASL and percentage of necrosis on subtraction have excellent performance for predicting CPN in HCC treated with locoregional therapy. In a previous study, DWI showed to be a significant predictor of complete tumor necrosis after TACE (AUC of 0.85), similar to subtraction (AUC of 0.82-0.89)4. DWI results in our study were disappointing, and conflicted with prior data4-6. After locoregional therapy, a treated HCC can increase in size secondary to intratumoral edema, hemorrhage, or necrosis7. Therefore, as expected, RECIST had no role in predicting CPN. This is the largest study validating mRECIST, EASL and subtraction against explant, confirming results from prior studies 8,9.
Conclusion: mRECIST, EASL and subtraction have excellent diagnostic value for predicting CPN in HCC treated with locoregional therapy. ADC should not be used for prediction of CPN in HCC post locoregional therapy.
Acknowledgements
No acknowledgement found.References
1. Eisenhauer E, Therasse P, Bogaerls J, et al. New response evaluation criteria in solid tumors: revised RECIST guideline version 1.1. Ejc Suppl 2008;6(12):13-13.
2. Lencioni R, Llovet JM. Modified RECIST (mRECIST) Assessment for Hepatocellular Carcinoma. Semin Liver Dis 2010;30(1):52-60.
3. Bruix J, Sherman M, Llovet JM, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL Conference. J Hepatol 2001;35(3):421-430.
4. Mannelli L, Kim S, Hajdu CH, Babb JS, Clark TWI, Taouli B. Assessment of Tumor Necrosis of Hepatocellular Carcinoma After Chemoembolization: Diffusion-Weighted and Contrast-Enhanced MRI With Histopathologic Correlation of the Explanted Liver. Am J Roentgenol 2009;193(4):1044-1052.
5. Taouli B, Koh DM. Diffusion-weighted MR Imaging of the Liver. Radiology 2010;254(1):47-66.
6. Yaghmai V, Besa C, Kim E, Gatlin JL, Siddiqui NA, Taouli B. Imaging Assessment of Hepatocellular Carcinoma Response to Locoregional and Systemic Therapy. Am J Roentgenol 2013;201(1):80-96.
7. Suzuki C, Jacobsson H, Hatschek T, et al. Radiologic measurements of tumor response to treatment: Practical approaches and limitations. Radiographics 2008;28(2):329-344.
8. Vouche M, Kulik L, Atassi R, et al. Radiological-Pathological Analysis of WHO, RECIST, EASL, mRECIST and DWI: Imaging Analysis from a Prospective Randomized Trial of Y90 +/- Sorafenib. Hepatology 2013;58(5):1655-1666.
9. Kim S, Mannelli L, Hajdu CH, et al. Hepatocellular Carcinoma: Assessment of Response to Transarterial Chemoembolization With Image Subtraction. J Magn Reson Imaging 2010;31(2):348-355.
Figures