4343
Using machine learning with dynamic exam block lengths to decrease patient wait time and optimize MRI schedule fill rate.1Department of Radiology, Stanford University, Stanford, CA, United States
Synopsis
MRI has advantages compared to other radiologic modalities in terms of tissue visualization, versatility, and lack of risks associated with ionizing radiation. However, cost of MRI is often the limiting factor favoring other modalities. Using historical scanner data and a Monte Carlo type discrete event simulation, we investigated how estimating exam length on the basis of patient demographics and dynamic block lengths affect mean patient wait times and schedule fill rate. In our simulation we are able to significantly lower mean patient wait times and optimize the schedule fill rate, which would theoretically result in lower cost per exam while enhancing patient satisfaction.
Purpose
MRI is often the safest and single most definitive diagnostic imaging test, but other imaging modalities are often used due to the relative higher cost of MRI. Given the high capital expense and fixed costs of MRI, as well as labor costs, the utilization rate of a scanner becomes a significant factor in the cost of an exam. Systematic assessment of scanner utilization rates in the United States and Canada have consistently shown rates around 70% of operational time1. Dead time, when the scanner is fully staffed but not imaging a patient, also results in unnecessary variable costs further driving the cost per exam performed. This is further complicated by the impact of perceived wait times on patient satisfaction2, limiting the opportunities for schedule optimization. While much research focus has aimed to decrease MR acquisition times3, comparatively little attention has been given to increasing scheduling efficiency and maximizing existing resources. The purpose of this study was to develop and evaluate a method to maximize scanner utilization while minimizing patient wait times.Methods
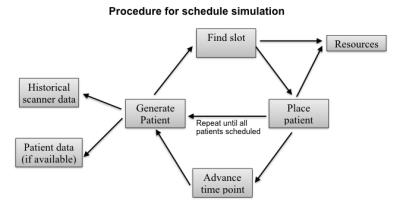
Scanner metadata for all exams performed on 8 inpatient and outpatient MRI scanners at our institution was collected from July 2015 to July 2016. Where available, patient demographics were collected as well. Next, a platform for Monte Carlo-type discrete event simulation was developed. In the first experiment, the simulation was initialized for 8 MRI scanners, operating for 16 hours a day, over a simulation horizon of 300 days. A block length of 60 minutes was fixed, as is customary at our institution. To initialize the simulation, 40% of the schedule slots were filled with randomly selected historic cases. Then simulated patients were randomly generated based on the historical data and scheduled according to the procedure depicted in Figure 1. Lastly, the schedule fill rate and wait time for each patient beyond the scheduled exam start time was calculated. A second experiment was set up with dynamic slot lengths determined at the time of scheduling. Using a feed-forward type neural network4, trained on a training data set, the upper bound length of the historical exam was predicted on the basis of patient demographics and used to schedule the exam. Again, schedule fill rates and wait times were calculated for each patient, taking into account the actual historical scan time compared to the predicted value. Both experiments were repeated 100 times and the results of schedule fill rate and mean patient wait times were compared using a student T-test. Excess exams for the dynamic block lengths, assuming an infinite patient pool, were also analyzed.Results
34611 unique exams were scanned during the study period composed of 525414 unique sequence acquisitions with 85593013 meta-data points collected.
Simulation results:
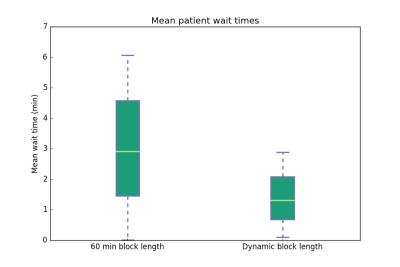
Mean patient wait times were significantly different (Fig 2) at 3.06 minutes (SD 1.82 minutes) with a fixed 60-minute block length compared with 1.38 minutes (SD 0.81 minutes) with dynamic slot length estimated with the feed-forward neural network (p<0.01*).
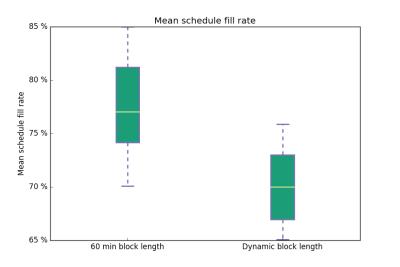
Mean schedule fill rates at constant throughput were significantly different (Fig 3) at 77.6% (SD 4.28) with a fixed 60-minute block length compared with 70.2% (SD 3.28) with dynamic slot length estimated with the feed-forward neural network (p<0.01*).
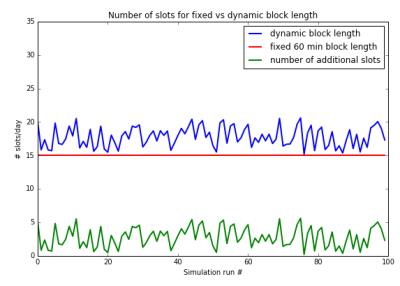
Assuming an infinite patient pool, 17.78 (SD 1.49) exams could be scheduled per day and scanner using the dynamic block lengths compared with the fixed 15 in the standard approach (Fig 4).
Discussion
Mean patient wait times can be reduced by using machine learning to estimate exam lengths on the basis of patient demographics. Further, dynamic block lengths result in a reduced schedule fill rate at constant throughput which would allow for additional exams to be performed. Assuming an infinite patient pool, this would result in an additional 2.78 exams scanned per day and scanner. Combined, these methods could allow for increased scheduling density while reducing mean patient wait times, ultimately resulting in lower cost per exam.
The use of historical scanner data and stochastic simulation may provide a realistic assessment of how changes to existing resources would affect different parameters, including patient wait times and schedule fill rate. However, the results of simulations are highly dependent upon the initial values and boundary conditions and thus more extensive investigation of parameters and implementation in a production environment will be necessary to demonstrate validity of these results.
Conclusion
Employing dynamic exam slot lengths set by a machine learning model could improve wait times while increasing scheduling capacity, potentially resulting in significant reduction in cost per exam.Acknowledgements
No acknowledgement found.References
1. Ariste R, Fortin G. Could MRI and CT Scanners Be Operated More Intensively in Canada? Health Policy. 2007;3(1):e113-20. http://www.ncbi.nlm.nih.gov/pubmed/19305746. Accessed November 5, 2016.
2. Holbrook A, Glenn H, Mahmood R, Cai Q, Kang J, Duszak R. Shorter Perceived Outpatient MRI Wait Times Associated With Higher Patient Satisfaction. J Am Coll Radiol. 2016;13(5):505-509. doi:10.1016/j.jacr.2015.11.008.
3. Hollingsworth KG. Reducing acquisition time in clinical MRI by data undersampling and compressed sensing reconstruction. Phys Med Biol. 2015;60(21):R297-322. doi:10.1088/0031-9155/60/21/R297.
4. Muelly M, Vasanawala SS. MRI Schedule Optimization through Discrete Event Simulation and Neural Networks as a means of Increasing Scanner Productivity. RSNA Annual Meeting 2016. Chicago, IL.
Figures