4258
Cardiovascular risk factors, cerebral blood flow, and cognitive functions: preliminary results in a community based study in Chinese elders1Singpare Bioimaging Consortium, Agency for Science Technology and Research, Singapore, Singapore, 2Department of Pharmacology, National University of Singapore, 3Memory Aging & Cognition Centre, National University of Singapore, 4Singapore Eye Research Institute, Singapore National Eye Center
Synopsis
Cerebral blood flow (CBF) is an important biomarker of the brain function and has been shown to correlate with cognitive performance in diseases. Since cardiovascular and metabolic complications are common in elders, to understand the influence of vascular confound in cognitive correlation, we investigated how cardiovascular risk factors may affect the relationship between cognitive functions and CBF in non-demented elders. We found that mean arterial blood pressure, haematocrit, blood cholesterol and glucose levels had significant negative effects on CBF. This suggests that cardiovascular risk factors shall be taken into consideration when analyzing CBF in aging, cognitive impairment, and neurodegenerative diseases.
Purpose
Cerebral blood flow (CBF) is an essential biomarker for the cerebrovascular function. Since it is also coupled with glucose metabolism, it could also be a marker of neural activity. Studies have suggested that lower CBF is associated with cognitive impairment 1, 2. Vascular diseases and metabolic syndromes are common in elders and dementia patients 3, but whether cognitive impairment is due to neurodegeneration or due to comorbid vascular and metabolic diseases is unknown. With growing use of CBF in aging and dementia research, it is important to determine the effects of common cardiovascular risk factors on CBF and cognition. The aims of this study were to understand the effects of cardiovascular risk factors on CBF, and then to examine the relationship between CBF and cognitive functions without confounding from those factors in a none demented elderly Chinese population from a community-based study.Methods
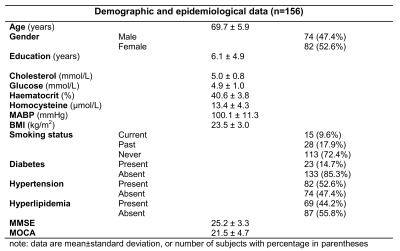
The study was approved by the Domain Specific Review Board (DSRB) of the National Health System, Singapore. 250 non-demented (based on neuropsychological tests and clinical assessments, as described previously 4) Chinese subjects from the on-going Epidemiology of Dementia in Singapore Study were recruited. All subjects underwent extensive examination including a questionnaire, physical examinations, blood tests, and cranial MRI. The Mini Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), the Informant Questionnaire on Cognitive Decline in the Elderly, and a formal neuropsychological battery were performed to assess mental functions including execution, attention, language, verbal memory, visual memory, visual construction, visual motor, and composite. After data quality control (removing poor images, missing data and outliers), 156 subjects (69.7±5.9 years old) were included in the statistical analysis.
MRI was performed on a 3T scanner (Trio, Siemens, Germany) with a 32 channel head array coil. Pseudo-continuous arterial spin labeling (PCASL) sequence with labeling time=1738ms, post-labeling delay=1500ms, and 2D gradient echo-EPI acquisition of TR/TE=4000/9ms, GRAPPA factor=3, voxel size=3x3x5mm3, and 23 pairs of averaging were acquired to measure CBF. T1-weighted 3D MPRAGE with 1x1x1mm3 voxel resolution was acquired for tissue segmentation and registration.
Image processing was carried out using FSL 5.0 (FMRIB Software Library, Oxford, UK), SPM8 (Statistical Parametric Mapping, UCL, UK), and in-house Matlab codes (The MathWorks, Inc., MA, USA). Structural MRI of each subject underwent brain extraction, bias field correction and segmentation. The PCASL data were preprocessed for motion correction, partial volume correction 5, quantification, quality control, spatial normalization and smoothing. Multiple linear regression models were tested with the mean CBF of the whole brain gray matter as the dependent variable, and cardiovascular risk factors as predictors while controlling for age, gender, and years of education. After a proper model was determined, it was applied to voxel-wise analysis, with multiple comparison corrected based on Gaussian random field theory with a significance threshold of p<0.05 at both voxel and cluster levels. Correlation between CBF and cognitive functions was tested with the demographic and risk factors controlled.
Results
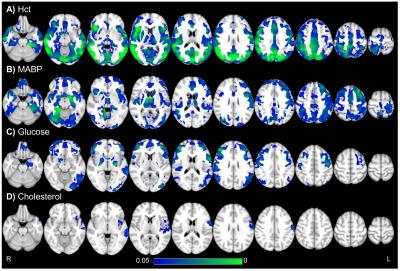
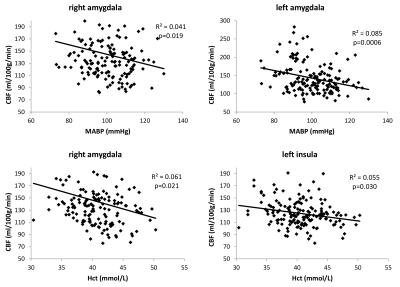
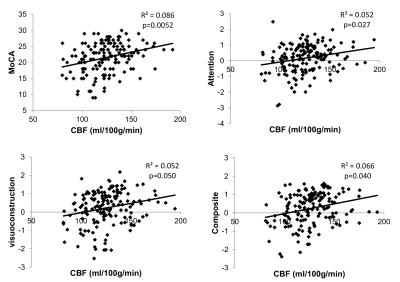
The demographic and epidemiological data are listed in Table 1. A regression model was determined with the mean arterial blood pressure (MABP), hematocrit (Hct), cholesterol, and glucose as significant contributing factors of CBF when controlling for age, gender, and education. Hct is strongly related to CBF in most regions of the temporal, parietal, and occipital lobes, while sparing most part of the frontal lobe; MABP is also associated with CBF in widespread regions, but to a lesser degree compared to Hct; Glucose mostly affects the frontal, temporal, and occipital cortices; Cholesterol is only correlated with part of the left temporal cortex (Fig.1). Figure 2 shows examples of the relationship in bilateral amygdala and left insular cortex. Positive correlation between CBF and cognitive scores including MoCA, attention, visuoconstruction, and composite is found in left insula (Fig.3).Discussion
Our findings of negative effects of Hct, MABP, cholesterol, and glucose on CBF are consistent with previous reports 6-9. The observed relationship between CBF and cognitive functions in the left insula confirmed its important role in integrating primary sensory information into high-order cognitive processing 10.Conclusion
CBF is negatively associated with Hct and MABP, and to a lesser degree with cholesterol and glucose, after controlling for age, gender, and education. This indicates that cardiovascular risk factors contribute to the variance observed in CBF. In addition, lower CBF in certain regions is associated with cognitive impairment after controlling for the demographic and cardiovascular factors. These preliminary results suggest that cognitive impairment may not be solely explained by vascular and metabolic diseases. Significant effect on insular suggests that network hub that integrate multiple information may be more vulnerable.Acknowledgements
This work was supported in part by the National Medical Research Council, Singapore (grant No R-184-006-184-511) and the intramural research fund of the Singapore Bioimaging Consortium, A*STAR, Singapore.References
1. Binnewijzend MA, Kuijer JP, Benedictus MR, et al. Cerebral blood flow measured with 3D pseudocontinuous arterial spin-labeling MR imaging in Alzheimer disease and mild cognitive impairment: a marker for disease severity. Radiology. 2013 Apr;267(1):221-30.
2. Wang Z, Das SR, Xie SX, et al. Arterial spin labeled MRI in prodromal Alzheimer's disease: A multi-site study. NeuroImage Clinical. 2013;2:630-6.
3. Hilal S, Saini M, Tan CS, et al. Cerebral microbleeds and cognition: the epidemiology of dementia in Singapore study. Alzheimer disease and associated disorders. 2014 Apr-Jun;28(2):106-12.
4. Hilal S, Ikram MK, Saini M, et al. Prevalence of cognitive impairment in Chinese: epidemiology of dementia in Singapore study. Journal of neurology, neurosurgery, and psychiatry. 2013 Jun;84(6):686-92.
5. Asllani I, Borogovac A, Brown TR. Regression algorithm correcting for partial volume effects in arterial spin labeling MRI. Magnetic resonance in medicine. 2008 Dec;60(6):1362-71.
6. Alosco ML, Spitznagel MB, Raz N, et al. Obesity interacts with cerebral hypoperfusion to exacerbate cognitive impairment in older adults with heart failure. Cerebrovasc Dis Extra. 2012 Jan;2(1):88-98.
7. Kusunoki M, Kimura K, Nakamura M, et al. Effects of hematocrit variations on cerebral blood flow and oxygen transport in ischemic cerebrovascular disease. J Cereb Blood Flow Metab. 1981;1(4):413-7.
8. Alosco ML, Gunstad J, Xu X, et al. The impact of hypertension on cerebral perfusion and cortical thickness in older adults. J Am Soc Hypertens. 2014 Aug;8(8):561-70.
9. Ayata C, Shin HK, Dilekoz E, et al. Hyperlipidemia disrupts cerebrovascular reflexes and worsens ischemic perfusion defect. J Cereb Blood Flow Metab. 2013 Jun;33(6):954-62.
10. Taylor KS, Seminowicz DA, Davis KD. Two systems of resting state connectivity between the insula and cingulate cortex. Hum Brain Mapp. 2009 Sep;30(9):2731-45.
Figures