4254
Medulloblastomas in adults: An MRI radiogenomic approach to an extremely rare disease1Radiology, University Hospital Bonn, Bonn, Germany, 2Institute for Diagnostic and Interventional Neuroradiology, University Hospital Wuerzburg, Wuerzburg, Germany, 3Institute for Neuropathology, University Hospital Bonn, Bonn, Germany, 4Wilhelm Sander-Therapieeinheit NeuroOnkologie and Clinic and Policlinic for Neurology, University Hospital Regensburg, Regensburg, Germany
Synopsis
Medulloblastoma in adults is very rare and shows prognostically relevant histological and genetic subtypes. Within a nation-wide multicenter study, pre-surgical MRIs of 28 cases were analysed to identify imaging biomarkers, which may be used to non-invasively predict these subtypes based on a radiophenotype. Molecular genetic subtypes SHH p53wt, WNT and non-WNT/non-SHH (Group 4) were significantly distinct in their relation to the 4th ventricle and lower rhombic limb, and extent of edema. Further imaging biomarkers could be identified that differentiate histological subtypes and nuclear-ß-catenin expression patterns. Imaging biomarkers were not congruent to markers identified in pediatric patients implying possible age-related differences.
PURPOSE
Medulloblastomas are rare in adult patients. The updated WHO classification of 2016 defines 4 histological and 5 genetic subgroups of medulloblastomas that only partially overlap. Histopathological and genetic profiles are known to influence the course of disease in children, and genetic subtype has shown to be linked to tumor location (1-5). The SHH-subtype constitutes the largest subgroup in adults with medulloblastoma. A single publication on children could correlate SHH subtype to a specific morphology on MRI (6). It is yet suspected that pediatric medulloblastomas are different from the adult variants.
This study is a first radiogenomic approach to identify MR imaging biomarkers of genetic subtypes in adult patients with medulloblastomas, which may facilitate pre-surgical tumor assessment and elucidate differences between adult and pediatric tumor variants.
METHODS
Between 2008 and 2014, 18 neuro-oncological centers recruited 30 patients with centrally confirmed and genetically sub-grouped medulloblastomas. Pre-surgical MRI datasets consisting of T1w, T2w, FLAIR and contrast-enhanced T1w sequences (CET1w) were available in 28/30 patients (10 women; age 23 – 53) and served as the basis for this retrospective analysis. Ethics approval was given for this subanalysis of the multicenter NOA-07 study (NCT01614132).
Three experienced neuroradiologists evaluated MR data based on 1. classical morphological characteristics (enhancement pattern, sharpness of tumor margins, T1 and T2 signal homogeneity and insensity compared to healthy tissue and hemorrhage) and 2. tumor volume and location (affection of the vermis, lateral hemispheres, the lower rhombic limb, N. VIII, the cerebellopontine angle and the brainstem), edema volume, Chang criteria on T2w and CET1w images and hydrocephalus (comp. fig. 1). Lesions were volumetrized with commercially available software (Intellispace Portal 5.0, Philips Healthcare) on CET1w and T2w images as well as perifocal edema on FLAIR images. Volume ratios were established between contrast-enhancing and T2-hyperintense volumes as well as T2-hyperintense volumes and edema.
With focus on genetic medulloblastoma subtypes SHH p53wt, WNT, and non-WNT/non-SHH (Group 4), genetic, histological and molecular information of the lesions (comp. fig. 1 for details) were analyzed with 2-sided Fischer and ANOVA testing to identify possible MR biomarkers. Findings were compared to biomarkers identified in the only radiogenomic medulloblastoma study in children (6).
RESULTS
In this cohort, only SHH p53wt, WNT, and non-WNT/non-SHH (Group 4) subtypes and no SHH p53mut or Group 3 tumors were diagnosed.
Genetic subtype: Several imaging biomarkers could be identified to differentiate molecular IHC-based subtypes (fig. 2). None of these markers corresponded to those identified by Perreault et al. in pediatric medulloblastomas. Nuclear-ß-catenin accumulating medulloblastomas (n=4) were 100% overlapping with WNT subtypes, were significantly smaller (P=0.03) and – different from non-accumulating tumors – never resulted in hydrocephalus or brainstem compression (P=0.02 and 0.03 respectively).
Histopathology: Perifocal edema was larger in the desmoplastic-nodular than in the classic histological subtype [median 8.67 (CI 5.66 – 11.69) vs. 2.28 (CI -1.08 – 5.65); all cm³; P=0.01]. Desmoplastic-nodular tumors were less frequently in contact with the 4th ventricle (4/15 vs. 7/13; P=0.04).
Apart from hemorrhage, none of the classical morphological MR markers (signal, enhancement, margins etc.) significantly differed between any of the genetic or histological subtypes.
DISCUSSION
We here define MRI biomarkers that may help to non-invasively distinguish three genetic and two histological subtypes from each other in adult medulloblastomas.
WNT and nuclear-ß-catenin overexpressing tumors, which could be linked to longer survival in medulloblastomas (1,7) and of which WNT is embryologically related to the lower rhombic limb, were smaller and differed from SHH p53wt or non-WNT/non-SHH (Group 4) lesions by lack of complicating factors like hydrocephalus.
Together, these biomarker findings illustrate how genetic polymorphisms may influence tumor morphology and possibly prognosis. Further research is needed to determine why smaller lesions result in early clinical manifestations and why pediatric biomarkers for genetic medulloblastoma subtypes differ from adult biomarkers identified in this study. A planned international prospective trial with larger patient numbers will be an opportunity to elaborate on these questions.
CONCLUSION
There are indicators that different genetic and histological subtypes of adult medulloblastoma can be preoperatively identified based on MRI imaging. These seem distinct from biomarkers in children. Concerted international efforts are needed to confirm these findings in larger collectives.Acknowledgements
No acknowledgement found.References
(1) Zhao F, Ohgaki H, Xu L, et al. Molecular subgroups of adult medulloblastoma: a long-term single-institution study. Neuro Oncol. 2016; 18(7):982-90.
(2) Fellay CN, Frappaz D, Sunyach MP, et al. Medulloblastomas in adults: prognostic factors and lessons from paediatrics. Curr Opin Neurol. 2011; 24(6): 626-32.
(3) Northcott PA, Hielscher T, Dubuc A, et al. Pediatric and adult sonic hedgehog medulloblastomas are clinically and molecularly distinct. Acta Neuropathol. 2011;122(2): 231-40.
(4) Remke M, Hielscher T, Northcott PA, et al. Adult medulloblastoma comprises three major molecular variants. J Clin Oncol. 201; 29(19):2717-23.
(5) Padovani L, Sunyach MP, Perol D, et al. Common strategy for adult and pediatric medulloblastoma: a multicenter series of 253 adults. Int J Radiat Oncol Biol Phys. 2007; 68(2):433-40.
(6) Perreault S, Ramaswamy V, Achrol AS, et al. MRI surrogates for molecular subgroups of medulloblastoma. AJNR Am J Neuroradiol. 2014; 35(7):1263-9.
(7) Phoenix TN, Patmore DM, Boop S, et al. Medulloblastoma Genotype Dictates Blood Brain Barrier Phenotype. Cancer Cell. 2016; 29(4):508-22.
Figures

Fig. 1 Study overview
Source data of the present study are pre-operative MRI data sets including contrast-enhanced T1w, T2 TSE and FLAIR sequences as well as tumor material for histopathological, genetic and molecular analyses retrieved during gross total tumor resection. Multiparametric MRI data of 28 patients was evaluated by 3 experienced neuroradiologists by classic morphological (1) and further volumetrical as well as location criteria (2).
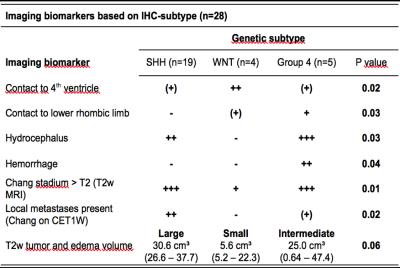
Fig. 2 Imaging biomarkers for medulloblastoma genetic subtype differentiation
SHH: sonic hedgehog subtype; WNT: wingless subtype, -: no positive cases; (+): < 25% positive cases; +: < 50% positive cases; ++: <75% positive cases; +++: ≥ 75% positive cases. Volumes stated as median and confidence intervals.