4250
A morphological classification of primary central nervous system lymphoma: new insights of the imaging analysis to facilitate treatment planning1Department of Radiology, Guangdong Academy of Medical Sciences/Guangdong General Hospital, Guangzhou, People's Republic of China, 2Russell H. Morgan Department of Radiology and Radiological Sciences, The Johns Hopkins University School of Medicine, Baltimore, MD, United States, 3Department of Mechanical and Biomedical Engineering, City University of Hong Kong, Hong Kong, People's Republic of China
Synopsis
A preliminary classification of primary central nervous system lymphoma (PCNSL) was reported based on the MRI radiographical features. We classified the 90 PCNSL patients based on the T1 contrast-enhanced MRI findings and assessed treatment responses. The goal is to provide some guidelines and additional information for diagnosis and treatment planning. We categorized these patients into four distinctive types of PCNSL according to the T1 findings and observed the treatment response rate, which we found the highest in type Ia. This could potentially facilitate the diagnosis and treatment plan of PCNSL in a routine clinical setting.
Purpose
Primary central nervous system lymphoma (PCNSL) is highly malignant non-Hodgkin’s lymphoma (NHL)1, which presents variable imaging appearances2. In this study, we classify PCNSL into four types based on T1 contrast-enhanced (CE) magnetic resonance imaging (MRI) findings and preliminarily investigated response rates (RR) in patients who received chemotherapy only.Methods
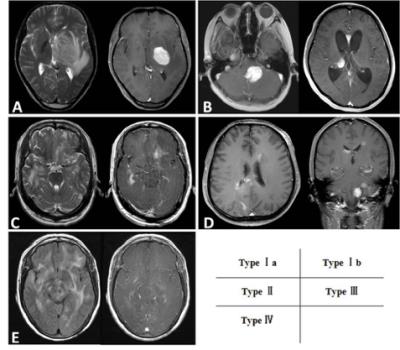
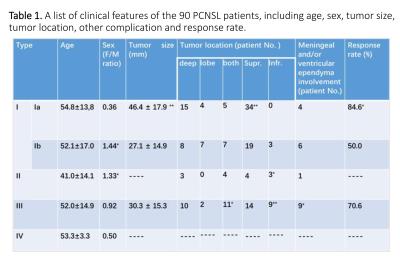
The clinical and radiological data of 90 primary cerebral lymphoma patients diagnosed between January 1, 2007 and December 31, 2015 were collected by three institutions in Guangzhou. All patients underwent radiological brain examination before needle or open biopsy using a 3.0T MRI system (PHILIPS Achieva, TX-Series, Netherlands). CE T1-weighted axial, sagittal and coronal images were acquired after intravenous administration of 0.1 mmol/kg gadopentetate dimeglumine (Gd-DTPA), using fast spin-echo T1WI, TR=570ms, TE=12ms, slice thickness=5mm, FOV=230mm. According to the MRI observations, we categorized the patients into (Fig.1 & Table 1.) (I) the mass type: cases present as a solid mass formation; (II) the infiltrative type: cases present as scattered lesions distributing in brain parenchyma with a patchy or streaky enhancement pattern, but without a mass formation; (III) the mixed type: cases present as both nodular and patchy enhancement lesions; and (IV) the nonenhanced type: cases present as diffusive, nonenhancing lesions without mass effect. The type I was further divided into the (Ia) monofocal type and the (Ib) multifocal type. Response to treatment was assessed on patients who received high dose methotrxate (HDMTX)-based chemotherapy only.Results
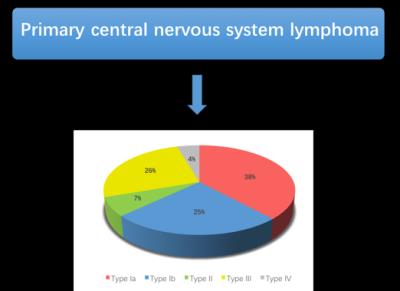
CE MRI of patients in the Type I showed a rather homogenous enhancement within a apparent tumor mass; the hyperintensity of Type II tumor appears more diffusive as compared to Type I. Type III showed a relatively smaller tumor mass and more diffusive lesions as compared to Type I. For Type IV, there was no isolated hyperintensity in the brain. Representative T1WI images for the types are shown in Fig. 1. All the clinical and observations are summarized in Table 1. Type II patients had a younger mean patient age of 42 , but no significant difference with other types. Type Ib and type II had a female preponderance (p<0.05). The largest mean tumor size was observed in the type Ia (p<0.001); infratentoria lesions were more commonly found in the type II and III (p<0.001); lesions of the type III appeared to involve both superficial and deep structures and the meninges or ventricular ependyma (p<0.05). Patients of type Ia were found to have a higher response rate (RR) (p<0.05) than type III (Table 1). The One-Way ANOVA and the Chi-square tests (χ2 test) were used to test the difference between the types of PCNSL.Discussion
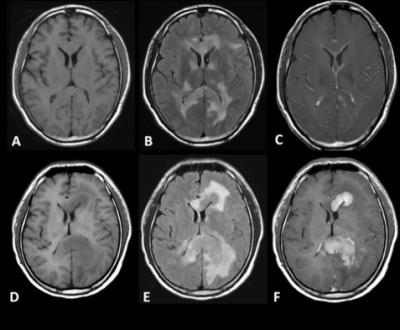
To the best of our knowledge, the present study is the first clinical image-based study to classify PCNSL into four types using CE MRI. We found that several clinical and radiological features were significantly different between the types. For instance, we found a lower age distribution in type II , suggesting age is an important factor that could affect the therapeutic outcome3 (Fig. 2). The mean tumor size is significantly larger in the type Ia. We speculated that symptoms appear earlier in patients of the type Ib and III, which could be ascribed to the damage over more brain functional areas by multiple lesions; patients of type III had an increasing trend to have infratentoria and deep structure lesions, and to involve the meninges or ventricular ependyma. This could be partially explained by the infiltrative nature of this tumor, which accounts for its ability to have distant disease. In addition, it is notable that the type IV as a variant type might be some kind of sentinel lesions that appear at a very early stage of PCNSL. (Fig. 3.) With respect to treatment response and follow-up, type Ia was found to have a high response rate and long-term disease control than other types and subtypes in our patient group.Conclusion
We developed a MRI-based classification for PCNSL, and found a relation between the types and the response rates (RR) to chemotherapy. This new classification could help clinicians and neuroradiologist to achieve a more comprehensive recognition and establish a precise diagnosis of PCNSL, and will potentially facilitate the decision-making of the optimal treatment plan of PCNSL patients in a routine clinical setting.Acknowledgements
This study is supported by the National Scientific Foundation of China (grant 81171329) and the Science and Technology Planning Project of Guangdong Province, China (grant 2014A020212244).References
1. Coulon A, Lafitte F, Hoang-Xuan K, et al., Radiographic findings in 37 cases of primary CNS lymphoma in immunocompetent patients. Eur Radiol. 2002 Feb;12(2):329-40.
2. Batchelor T, Loeffler JS. Primary CNS lymphoma. J Clin Oncol. 2006 Mar 10;24(8):1281-8.
3. Thiel E, Korfel A, Martus P, et al., High-dose methotrexate with or without whole brain radiotherapy for primary CNS lymphoma (G-PCNSL-SG-1): a phase 3, randomised, non-inferiority trial. Lancet Oncol. 2010 Nov;11(11):1036-47.
Figures