4233
Detecting treatment response of a novel immune stimulator in an animal model of glioblastoma with conventional and cell tracking MRI1Radiology, University of Calgary, Calgary, AB, Canada, 2Clinical Neuroscience, University of Calgary
Synopsis
Glioblastoma Multiforme (GBM) is an aggressive brain cancer. Immunotherapy is a promising avenue of exploration for treatment of GBM. We discovered a new drug capable of stimulating innate immunity and showed that it is able of reducing tumor growth in a mouse model of GBM. We used ultrasmall iron oxide nanoparticles (USPIO) to track the migration of stimulated immune cells and showed that this drug related response can be detected with as little as 7 days of treatment. MRI tracking of immune cells using USPIO is a promising tool that can be easily translated into the clinical setting.
Purpose
Glioblastoma Multiforme (GBM) is an aggressive brain cancer. It is believed that the poor prognosis1 is caused by stem-like cells called brain tumor initiating cells (BTIC). BTIC’s are chemo and radiation resistant2, and they are thought to be responsible for tumorigenesis3. It has been shown that Amphotericin B (Amp B) is capable of stimulating the innate immune system (monocytes) to suppress BTICs4. However, Amp B is not well tolerated in humans. In a large screening study, we found a drug capable of stimulating the immune system that is well tolerated by patients. A publication is being prepared and so the drug name is under embargo. We will name the drug at ISMRM. This study uses an ultrasmall iron oxide nanoparticle (USPIO) MRI monocyte tracking method which we developed5 to show that this drug does stimulate the innate immune system, and that monocytes are trafficked to the tumor to achieve tumor control.Methods
In study 1, we used a cell tracking method we developed5 to determine the drug’s effects on monocytes. We implanted 10,000 human BTICs into the right striatum of 8-10 week old severe combined immune-deficient (SCID) mice6. Drug (n=4) or vehicle (n=4) treatment was started 35 days after tumor implantation and lasted at least 7 days. MRI was performed with a 9.4T MRI (Buker) and a helium cooled cryocoil. A baseline multiecho gradient echo (MEGE) sequence was performed (TR/TE/α = 1500ms/3.1, 7.1, 11.1, 15.1, 19.1 ms/30o, voxel size =0.075 mm x 0.075 mm x 0.35 mm). Ferumoxytol (30mg/kg, 100 uL) was injected in the tail vein. The MEGE sequence was repeated 24 hours post ferumoxytol injection. Perfusion fixation was performed. DAB-enhanced Perl’s stain was used for iron and Iba1 for monocyte/macrophages. One slide from each animal was presented to a blinded observer, who ranked the amount of Iba1 staining within the tumor. A rank sum analysis was then carried out.
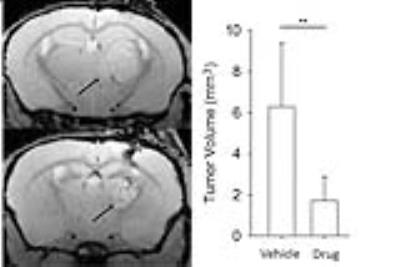
To validate the anti-tumor effects of the drug, drug (n = 5) or vehicle (n = 5) treatment was initiated 7 days after tumor implantation. Anatomical MRI was performed 42-45 days post implantation. A FLASH sequence (TR/TE/α = 1000ms/6.5ms/60o, voxel = 0.075 x 0.075 x 0.25 mm) was used.
All MRI analysis was performed using ImageJ
Results
In the drug treated animals, there was a greater darkening on the T2*w image and a greater reduction in T2* within the tumor compared to vehicle controls (p<0.001; Figure 1). The drug also significantly reduced tumor growth (p<0.01; Figure 2). There was more Iba1 (macrophage/microglia) staining in treated animals compared to vehicles as shown visually and with a “blinded” reader ranking the images for extent of staining (p<0.05; Figure 3). In addition, we showed that the Iba1 stain (monocyte/macrophages) appears to be co-localized with the DAB enhanced Perl’s iron stain (Figure 4).Discussion
Treatment with the innate immune stimulating drug significantly reduced the tumor growth, indicating that the drug provide excellent tumor control. The significant decrease in T2* in the tumor after ferumoxytol injection, and the co-localization of monocyte/macrophage staining with iron staining supports the premise that stimulated monocytes are engulfing the ferumoxytol and migrating into the tumor. Ferumoxytol does not cross the BBB by other mechanisms as the T2* does not decline in vehicle controls. By labeling monocytes using ferumoxytol enhanced MRI, we were able to observe the efficacy of this drug after only 7 days of treatment instead of having to wait weeks to detect changes in tumor size. Ferumoxytol is a safe agent that has been extensively used in the patient population and is clinically approved to treat anemia.Conclusion
We used a drug that stimulates innate immunity to reduce tumor growth in vivo and showed that USPIO based cell tracking could be used to detect infiltration of stimulated monocytes to the brain tumor. This MRI monocyte tracking method has not been done by other groups in brain tumors, and it shows excellent promise as a technique for translation to human studies to detect the efficacy of drugs that stimulate the innate immune system to control brain cancer.Acknowledgements
This study was funded by the Alberta Innovates Health Solutions - Alberta Cancer Foundation, Branch Out Neurological Foundation Graduate Studentship, and Alberta Innovates Health Solutions Graduate Studentship.References
1. Stupp, R., et al., Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med, 2005. 352(10): p. 987-96.
2. Hardee, M.E., et al., Resistance of glioblastoma-initiating cells to radiation mediated by the tumor microenvironment can be abolished by inhibiting transforming growth factor-beta. Cancer Res, 2012. 72(16): p. 4119-29.
3. Singh, S.K., et al., Identification of human brain tumour initiating cells. Nature, 2004. 432(7015): p. 396-401.
4. Sarkar, S., et al., Therapeutic activation of macrophages and microglia to suppress brain tumor-initiating cells. Nat Neurosci, 2013. 17(1): p. 46-55.
5. Yang, R., et al., MRI monitoring of monocytes to detect immune stimulating treatment response in brain tumor. Neuro Oncol, 2016.
6. Kelly, J.J., et al., Proliferation of human glioblastoma stem cells occurs independently of exogenous mitogens. Stem Cells, 2009. 27(8): p. 1722-33.
Figures