4204
Intraspinal bronchogenic cyst: Series of case reports and literature review1Imaging Medical, The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, People's Republic of China
Synopsis
The purpose of this study was to provide a deeper knowledge of clinical presentation, imaging diagnosis, differential diagnosis and the management of the intraspinal bronchiogenic cysts. We retrospectively studied three cases of SBCs which were registered in our department and analyzed eight case reports which were all published in English. The SBCs can occur anywhere in the spinal canal, but they are more likely to present at the cervical canal and might be along with some developmental malformations of spine. We emphasize the role of MRI findings in the diagnosis before surgery. It is recommended that the lesion should be removed as completely as possible on the premise of protecting the spinal cord from being injured.
Purpose
Spinal bronchogenic cysts (SBCs) are rare congenital lesions which are lined with pseudostratified ciliated columnar epithelium 1. The clinical and imaging characteristics and treatment of SBCs are not well known. It is difficult to make a right diagnosis before surgery due to its extremely low morbidity and non-typical symptoms, signs and imaging findings Advances in MRI have led to an increased understanding of SBCs, although such cysts may be often misdiagnosed as arachnoid and epidermoid cysts 2. We studied three cases of SBCs retrospectively, which were registered in our department and analyzed eight case reports which were all published in English, focusing on providing a deeper knowledge of SBCs.Methods
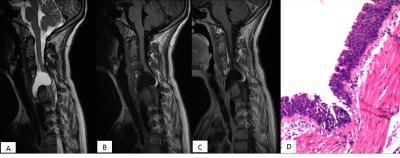
Three patients with SBCs registered in our department were retrospectively reviewed. Eight reported SBCs cases published from 1992 to 2015 were enrolled in our study. Imaging diagnosis was confirmed by MRI, CT, and computed tomography angiography (CTA). The detailed MRI characteristics such as location, shape, size, margin, signal intensity were analyzed. All of our patients and reviewed cases had undergone surgical resection and the final diagnosis was made by pathological examination.Results
Five lesions were located at the cervical spinal canal, while a thoracic location occurred in three patients. Two cysts were located at lumbar and sacral spinal canal. One lesion was stretching to extraspinal space through the intervertebral foramen. Most patients presented with pain in the limbs and back. Six cysts presented with homogenous hyperintense on the T2WI and hypointense on T1WI, and only one case showed heterogeneous hyperintense on T2WI and hypointensity on T1WI. Two cases had lipomatous tissue adhered to the caudal end of the cystic mass which presented with high signal on both T1WI and T2WI. Seven lesions were partially removed because of the adhesions to the nearby spinal cord. All reported cases had no recurrence in the later follow-up.Discussion
Although the SBCs were rare, it should not be ignored by radiologists. It can occur anywhere in the spinal canal, but they are more likely to present at the cervical canal and might be present along with some developmental malformations of the spine. The signal intensity on MRI was correlated with cystic fluid traits to a large extent. Some lipomatous signal was observed in two cases 3. Whether the sign is specific for SBCs, it may need more literature reviews and studies. Some research established that the complete excision of the wall by aspiration and ideal marsupialization were closely associated with a favorable prognosis 4.Conclusions
We emphasize the role of MRI findings in the disease diagnosis before surgery.Acknowledgements
Xueying Ma and Dun Ding drafted the manuscript. Xueying Ma, Dun Ding and other authors were responsible for collecting the cases.References
1. Rao GP, Bhaskar G, Reddy PK. Cervical intradural extramedullary bronchiogenic cyst. Neurology India1999. p. 79-81.
2. Wang MY, Levi AD, Green BA. Intradural spinal arachnoid cysts in adults. Surg Neurol 2003;60(1):49-55; discussion -6.
3. Baumann CR, Konu D, Glatzel M, Siegel AM. Thoracolumbar intradural extramedullary bronchiogenic cyst. Acta Neurochir (Wien) 2005;147(3):317-9; discussion 9.
4. Tucker A, Miyake H, Tsuji M, Ukita T, Ito S, Matsuda N, et al. Neurenteric cyst of the lower clivus. Neurosurgery 2010;66(1):E224-5.
Figures