4195
Expanding the Role of the Rapid Sequence MRI in Pediatric Neuroimaging1Phoenix Children's Hospital, Phoenix, AZ, United States
Synopsis
The Image Gently campaign has resulted in increased awareness of radiation risks in the pediatric population. A major effect of this is a reduction in computed tomography in pediatric hospitals. While MRI may be able to achieve many of the goals of CT, risks related to sedation and the need for increased resources to perform sedated MRI must also be considered for children with conditions known to require follow-up imaging. In cases where children have external ventricular shunts in place over a long term, rapid sequence MRI has been well-described in its role to assess ventricular size while avoiding both ionizing radiation and sedation. Here we describe the use of our version of the rapid sequence MRI to assess additional indications, as more than half of the patients undergoing this study in our facility do not have indwelling ventricular shunt catheters at the time of imaging. Limitations of this technique are also discussed.
Purpose
The purpose of this exhibit is to examine the advantages and limitations of expanding the spectrum of neurologic indications regarding the use of rapid sequence magnetic resonance imaging in the pediatric population.Outline of Content
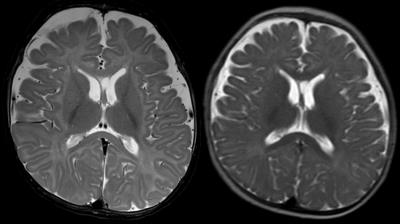
Rapid sequence MRI has long been employed in the evaluation of ventricular size among pediatric patients requiring assessment and reassessment of shunt function [1]. This technique, which generally relies on single-shot acquisition methods, has also been shown to result in excellent visualization of the intracranial hardware [2] while significantly decreasing radiation exposure in this sensitive patient population who would otherwise require computed tomography [3].
Concern for neurotoxicity of some anesthetics and sedatives has prompted clinicians to limit anesthesia in children under 3 years of age [4]. Given the time requirement of conventional magnetic resonance imaging, standard MRI techniques can result in significant motion-related artifact and subsequent degradation of detail. Rapid sequence MRI, when employed appropriately, can thus avoid sedation-related risks in addition to the biologic risks associated with radiation exposure in the pediatric population.
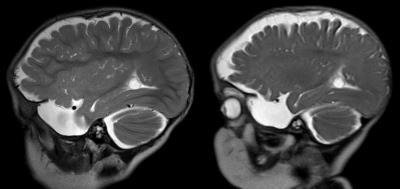
Our institution uses an expanded form of the rapid sequence MRI which not only includes single-shot heavily T2-weighted acquisition in 2 planes but also employs a diffusion weighted sequence to assess for ischemia, fast steady-state gradient recalled-echo in 2 planes for evaluation of intracranial hardware, and rapid coronal FLAIR to examine extra-axial spaces. This acquisition set has the advantage of quick image generation with sufficient standardization to aid in the diagnosis in an array of clinical concerns.
To investigate the role that this technique has had on clinician ordering practices at our pediatric facility, 100 consecutive rapid sequence brain MRI's were studied with respect to indication and performance.
While the original conception of the rapid sequence MRI was aimed at the evaluation of shunted hydrocephalus, only 41% of examinations were ordered on patients with a shunt in place at the time of imaging. In an additional 17%, the noted reason for exam specifically referenced ventricular size assessment.
Interestingly, 13% of exams were ordered to assess the size of intracranial cysts, and an additional 7% of indications specifically referenced measuring the evolving size of extra-axial fluid collections. A clinical concern for stroke was stated in 8% of studies. A prenatal question of Dandy-Walker malformation had been raised in 2% of the patients.
In 12 of the 100 exams, the rapid sequence MRI was the first neurologic imaging study ordered, 9 of which were intended to screen for possible hydrocephalus or stroke. A reasonable conclusion is that some clinicians have converted this test into a screening exam, a practice which should be recommended with caution. As such, an appropriate disclaimer regarding the inability to assess parenchymal detail is in order when reporting.
In 96% of the examinations, the clinical concern was specifically referenced in the impression. In the remaining 4%, the report stated that the ventricular size was normal, however, rapid sequence technique was insensitive to address the clinical question. In none of the 100 studies did the radiologist state that assessment of the clinical question was impossible due to motion-related artifact.
While the size of intracranial fluid collections can often be tracked using this technique, a word of caution is in order when trying to use MRI to age hemorrhagic products, as would be the case in suspected abusive head trauma. As such, rapid sequence MRI is intended for use in known causes of extra-axial fluid accumulation such as surgical intervention. Standard imaging techniques should be employed when a primary intracranial diagnosis remains in question.
Summary
Through the appropriate sequence planning and education of ordering clinicians, expanding the role of rapid sequence MRI can be a useful tool to safely address common clinical conditions in children without the need for sedation or extended scanning times.Acknowledgements
No acknowledgement found.References
1. Ashley WW Jr, McKinstry RC, Leonard JR, Smyth MD, Lee BC, Park TS. Use of rapid-sequence magnetic resonance imaging for evaluation of hydrocephalus in children. J Neurosurg 2005;103(2 Suppl):124-130.
2. Miller JH, Walkiewicz T, Towbin RB, Curran JG. Improved delineation of ventricular shunt catheters using fast steady-state gradient recalled-echo sequences in a rapid brain MR imaging protocol in nonsedated patients. AJNR Am J Neuroradiol 2010;31:430-435.
3. Koral K, Blackburn T, Bailey AA, Koral KM, Anderson J. Strengthening the argument for rapid brain MR imaging: estimation of reduction in lifetime attributable risk of developing fatal cancer in children with shunted hydrocephalus by instituting a rapid brain MR imaging protocol in lieu of head CT. AJNR Am J Neuroradiol 2012;33:1851-1854.
4. Rappaport BA, Suresh S, Hertz S, Evers AS, Orser BA. Anesthetic neurotoxicity--clinical implications of animal models. N Engl J Med 2015;372:796-797.
Figures