4182
Intraoperative Arterial Spin Labeling – feasibility and first results1Clinic for Radiology and Neuroradiology, University Hospital Schleswig-Holstein, Kiel, Germany, 2Clinic for Neurosurgery, University Hospital Schleswig-Holstein, Kiel, Germany, 3Clinic for Neurosurgery, University Hospital Göttingen, Göttingen, Germany, 4Tomographic Imaging Department, Philips Research, Hamburg, Germany, 5Medizinisch Radiologisches Institut, Zurich, Switzerland
Synopsis
Performing MRI studies in an intraoperative setting is generally limited due to hardware and patient positioning restrictions. Structural imaging alone might not be sufficient to gather all required information. The goal of this study was to implement pseudo-continuous ASL in the intraoperative neurosurgical setting with limited hardware available and compare the images with measurements obtained pre-, and postoperatively on different clinical MRI scanners. The first application in a patient shows the potential of intraoperative ASL imaging with regards to visualizing residual tumor mass already during the surgical intervention in similar image quality.
Introduction
The use of imaging devices in an intraoperative setting may help surgeons to complete procedures with improved safety, efficiency and clinical outcome. Performing MRI studies in an intraoperative setting is generally limited due to hardware and patient positioning restrictions and performing only structural imaging might not be sufficient to gather all needed information (e.g. grade of resection). One parameter is cerebral perfusion, as the knowledge about it might increase diagnostic confidence about malignity and progression of tumors [1]. One method to visualize perfusion is Arterial Spin Labeling (ASL), which is a non-invasive method that it uses blood as endogenous contrast agent. Therefore no external contrast agents have to be applied. The goal of this study was to apply pseudo-continuous ASL in the intraoperative neurosurgical setting and analyze the results obtained from three MRI machines with different hardware set-ups to optimize and compare image quality pre-, intra- and postoperatively.Materials and Methods
In this study, 10 healthy volunteers (6 women, 4 men, mean age 31.4 years) underwent scanning on three MRI machines with different hardware setup (all from Philips Healthcare, Best, The Netherlands) including a 3T (Achieva series) scanner equipped with a 32-channel receive head coil and a 1.5T (Achieva series) scanner with a 6-channel head coil, located in the department of radiology and neuroradiology and another 1.5T scanner (Intera series) equipped with two one-channel circular coils in the operating room (OR) of the neurosurgical department. The study was approved by the local ethical committee. The volunteers underwent ASL scanning within one hour in each of the three scanners. Scan parameters included: 1800ms labeling duration and post labeling delay, 2D multislice EPI scanning with 3.6x3.5x5mm³ resolution, TR/TE: 2616/13ms. To account for lower signal contribution of the 1.5T scanners and the reduced number of receive channels, the number of label and control pairs was increased from 20 pairs at 3T, 30 pairs at 1.5T with 6 channels and 40 pairs at 1.5T with 2 channels. The resulting images were quantified using the algorithm described in [2] and compared regarding their mean CBF values. As a statistical measure, the correlation coefficient was used. Additionally, one patient suffering from glioblastoma was included who underwent pre-, and postoperative scanning on the 3T and intraoperative scanning in the operating theater within three daysResults and Discussion
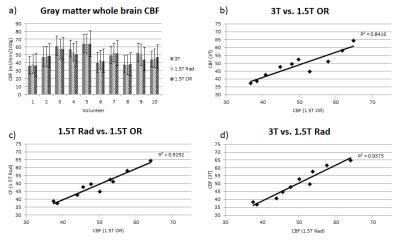
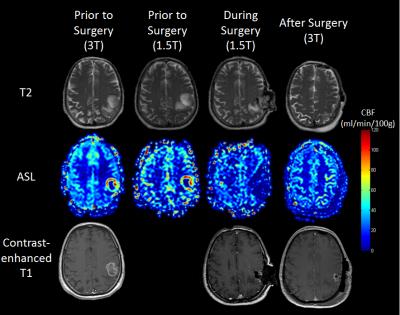
Rather high inter-individual deviations in CBF values were found within the volunteer cohort (Figure 1a). The mean CBF values obtained on the scanners were 49.53 ± 9.72 for 3T, 49.15 ± 8.28 for 1.5T in the radiology department, and 48.65 ± 8.43 ml/min/100g on 1.5T in the neurosurgical setting. The differences between the scanners for each volunteer were minimal and show excellent correlation (Figure 1b-d). The patient scan shows a total resection after clearly delineating the glioblastoma in the ASL images, which could also be verified by established morphological MRI using contrast agent application (Figure 2). Figure 2 also shows that image quality subjectively differs in each scanner, depending on field strength and number of receive channels but this had no effect on the diagnostic quality in this case. The injection of the contrast agent intraoperatively did not seem to influence the post-operative ASL scan, as this scan is usually performed the day after the surgery, however, consideration is required in further studies.Conclusion
This preliminary study shows the comparability of the results obtained by MRI machines with different field strengths and available hardware. The first application in a patient shows the potential of intraoperative ASL imaging with regards to visualizing residual tumor mass already during the surgical intervention. Based on these results, future studies with patients suffering from various cerebral diseases (e.g. tumors, metastasis, etc.) are planned.Acknowledgements
No acknowledgement found.References
[1] Law M. et. al. Radiology 2006;238:658-67
[2] Alsop D et. al. Magn Reson Med 2014;73:102-16
Figures