3899
Impact of MR-based Motion Correction on clinical PET/MR data of patients with thoracic pathologies1Erwin L. Hahn Institute, University Duisburg-Essen, Essen, Germany, 2High Field and Hybrid MR Imaging, University Hospital Essen, Essen, Germany, 3Department of Nuclear Medicine, University Hospital Essen, Essen, Germany, 4Department of Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Essen, Essen, Germany, 5Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
A new PET/MR method for MR-based motion correction of PET data was set up and evaluated in a clinical study to assess the potential gain of significance and visibility of lesions in the thorax for a free-breathing patient. The new method (MoCo) was applied to 20 patients and compared to reconstructions of a single respiratory state (gated) and the total non-corrected (static) dataset. Having a comparably high statistical confidence like the static PET imagery, the motion-corrected reconstruction shows superior image quality with sharper depiction of moving lesions and thus may facilitate the diagnosis of thoracic pathologies in routine PET/MR applications.
Purpose
A new method for MR-based motion correction of PET data in the context of integrated PET/MR was implemented and evaluated in a clinical study on 20 patients. The potential gain in thoracic lesion visibility was assessed with a motion-correction protocol during free breathing. Non-motion-corrected standard PET reconstructions served as reference standard.Methods
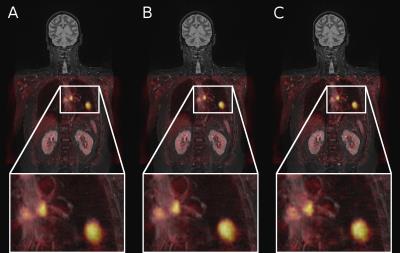
Twenty patients (mean age 64.6 ± 8.8 yrs, 13 male, 7 female) with various PET active lesions in the thorax underwent a routine clinical imaging protocol on an integrated PET/MR system (Biograph mMR, Siemens Healthcare. Erlangen, Germany) using 18F-FDG as radiotracer. The imaging protocol was extended by an additional free-breathing self-gated acquisition of MR data that is used to model the motion of the thorax during breathing1-4. PET data was recorded in List-Mode along with the scan for a duration of 5-10 min and subsequently was reconstructed in three different ways that included (A) all data irrespective of the underlying motion (static), (B) conventional gating, i.e. selection of only particular data that belong to one specific respiratory state (gated) and (C) data binning to different respiratory phases which was retrospectively mapped to a single motion state using the deformation fields as obtained by analysis of the underlying MR images (Motion Correction, MoCo). Following PET data reconstruction, all data sets were read by an experienced radiologist and a nuclear medicine specialist in consensus, evaluating lesion visibility and image noise levels on a 4- and 3-point ordinary integer scale (visibility: 4 – very detailed ... 1 – non-diagnostic; noise: 3 – low noise level ... 1 – high noise level), respectively. Moreover, maximum and mean standardized uptake values (SUVmax and SUVmean) were obtained along with their corresponding values in the liver as a reference.Results
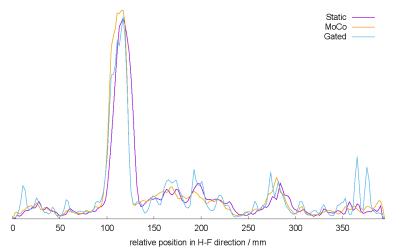
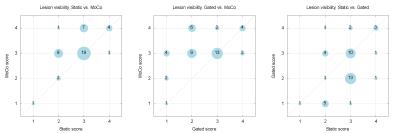
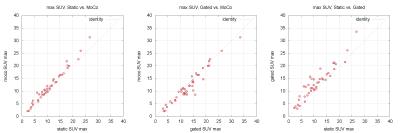
All 20 patients tolerated the PET/MR imaging protocol well. Altogether, 43 lesions were evaluated in this study. Fig. 1 and 2 provide a visual comparison between fused PET/MR images as reconstructed by each presented method. The exemplary line profile in Fig. 3 along the transverse main motion direction supports an enhancement in sharpness over the static reconstruction. With a mean visibility score of 3.19 ± 0.63, the motion-corrected PET data received a similar (26 cases) or higher score (16 cases) than the static PET data with a mean score of 2.81 ± 0.66 (see Fig. 4). When comparing MoCo to the gated reconstruction, this finding still holds with 41 lesions being better (23 cases) or equally (18 cases) represented in their respective visibility (mean visibility score for the gated method was 2.47 ± 0.93). The noise level evaluation showed a clear trend in favor of the static and MoCo approach with a perfect match of scores (Pearson correlation r = 1, mean score 2.95 ± 0.21), while the PET images obtained from the gated reconstruction suffered significantly from noise (mean score 1.27 ± 0.46). When correlating the SUVs of all methods to each other, a close distribution along the identity was observed particularly for the SUVmean values (Pearson correlation coefficients: static vs. MoCo r = 0.9884, static vs. gated r = 0.9850, gated vs. MoCo r = 0.9938). Furthermore, the SUVmax values are slightly elevated for the gated method compared to MoCo and static approach, respectively, while the MoCo PET data shows a mean deviation of +1.02 ± 1.22 from the corresponding values in the static PET data (Fig 5).Discussion and Conclusion
The expectation of a sharper representation of lesions in the images compared to a pure static reconstruction is confirmed for the new MoCo and the gated approach within a first visual impression. Due to the nature of the gated reconstruction approach, much fewer counts are taken into account and thus reduce significance while introducing a high level of noise into the PET image data. Since signal intensity is smeared out with motion, the obtained mean SUVs in the case of non-corrected motion are slightly lower than with applied motion correction. Oppositely, the high noise level of the gated method introduces a rather major spread of the SUVmax values as compared to the static and motion-corrected data. In conclusion, the newly presented motion-corrected PET reconstruction renders superior in comparison to its alternatives with approximately the same high statistical confidence like the static approach, yet a better depiction of details. This may facilitate detection of small lesions particularly in moving body parts such as the thorax, liver, and abdomen via PET/MR and provides a viable option that may potentially be extended to e.g. cardio-vascular applications in the future.Acknowledgements
This work was supported by a research agreement between the University Hospital Essen and Siemens Healthcare GmbH.References
1.
Grimm R, Fürst S,
Dregely I, et al. Self-gated Radial MRI for Respiratory Motion
Compensation on Hybrid PET/MR Systems, MICCAI Proceedings 2013;16(Pt 3):17-24
2. Würslin, Schmidt, Martirosian, et al. Respiratory motion correction in oncologic PET using T1-weighted MR imaging on a simultaneous whole-body PET/MR system. JNM 2013;54(3)464-71
3. Guérin B, Cho S, Chun SY, et al. Nonrigid PET motion compensation in the lower abdomen using simultaneous tagged-MRI and PET imaging. Medical Physics 2011;38(6):3025-38
4. Chun SY, Reese TG, Ouyang J, et al: MRI-based nonrigid motion correction in simultaneous PET/MRI, JNM 201;53(8):1284-91
Figures